Lessons for the Long Term
Investigation into the Ministry of Long-Term Care’s oversight of long-term care homes through inspection and enforcement during the COVID-19 pandemic.

Table of contents
Show
Hide
Lessons for the Long Term
Investigation into the Ministry of Long-Term Care’s oversight of long-term care homes through inspection and enforcement during the COVID-19 pandemic
Paul Dubé
Ombudsman of Ontario
September 2023
Office of the Ombudsman of Ontario
We are
An independent office of the Legislature that resolves and investigates public complaints about services provided by Ontario public sector bodies. These include provincial government ministries, agencies, boards, commissions, corporations and tribunals, as well as municipalities,
universities, school boards, child protection services and French language services.
Land acknowledgement and commitment to reconciliation
The Ontario Ombudsman’s work takes place on traditional Indigenous territories across the province we now call Ontario, and we are thankful to be able to work and live on this land. We would like to acknowledge that Toronto, where the Office of the Ontario Ombudsman is located, is the traditional territory of many nations, including the Mississaugas of the Credit, the Anishnabeg, the Chippewa, the Haudenosaunee, and the Wendat peoples, and is now home to many First Nations, Inuit and Métis peoples.
We believe it is important to offer a land acknowledgement as a way to recognize, respect and honour this territory, the treaties, the original occupants, their ancestors, and the historic connection they still have with this territory.
As part of our commitment to reconciliation, we are providing educational opportunities to help our staff learn more about our shared history and the harms that have been inflicted on Indigenous peoples. We are working to establish mutually respectful relationships with Indigenous people across the province and will continue to incorporate recommendations from the Truth and Reconciliation Commission into our work. We are grateful for the opportunity to work across Turtle Island.
Contributors
Director, Special Ombudsman Response Team
- Domonie Pierre
Lead Investigators
- Rosie Dear
- Chris McCague
Investigators
- Emily Ashizawa
- Armita Bahador
- Richard Francis
- Alex Giletski
- Yvonne Heggie
- Carmen Kallideen
- John O’Leary
- Karyna Pavlenko
- Dahlia Phillips
Early Resolution Officers
- Angela Alibertis
- Olivia Hannigan
- Claudia Rios
- Kirsten Temporale
Senior Counsel
- Robin Bates
General Counsel
- Laura Pettigrew
Press Conference
Executive Summary
1 Few lives have remained untouched by the COVID-19 pandemic. When this novel coronavirus emerged as a global pandemic in March 2020, many naively thought that it would take a few weeks to “flatten the curve” and then life would continue as normal. However, that initial optimism soon faded as new COVID-19 variants arose and wave after wave swept through the province. Up to May 5, 2023, when the World Health Organization declared an end to the global emergency status for COVID-19, the virus had claimed the lives of more than 15,000 Ontarians.
2 While each loss of life is a tragedy, certain high-risk and vulnerable populations were disproportionately impacted by the virus, including those working and living in Ontario’s long-term care homes. Between the start of the pandemic and April 2022, 4,335 long-term care residents and 13 staff members died from COVID-19, and more than 41,000 were infected.[1] The first wave took a particularly heavy toll at a time when little was known about the disease, or how to best contain or treat it. Close to 2,000 COVID-related deaths in the long-term care sector occurred during the first wave of the pandemic, from January 15, 2020 until August 2, 2020.
3 This report stems from the devastating “first wave” of the COVID-19 pandemic. It was a time when the world was still coming to terms with the rapidly spreading virus – and before Ontario’s response to the crisis was subjected to a series of reviews and recommendations for improvement. Since then, many significant changes have been made to shore up the province’s capacity to weather a similar emergency in future – but much more needs to be done to address the serious lapses in oversight I have detailed in this report. My investigation and recommendations have focused on evidence not revealed in other reviews, and the remedial action necessary to ensure Ontario is better prepared and its residents better protected when future crises arise.
4 Ontario has more than 600 long-term care homes, collectively comprising nearly 80,000 resident beds. Long-term care homes provide access to 24-hour nursing and personal care in a home-like environment. These services are crucial to maintaining the health and dignity of residents, the vast majority of whom need extensive help with daily activities such as getting out of bed, eating or toileting, and experience some form of cognitive impairment or neurological disease. Long-term care homes are overseen by the Ministry of Long-Term Care, which is responsible for licensing the homes, receiving complaints, conducting compliance inspections, and taking enforcement action if a home is not complying with legal requirements. In addition to the Ministry of Long-Term Care, other organizations oversee long-term care homes, including the Ministry of Health, local public health units, and Ontario’s Patient Ombudsman.
5 As the first wave of the pandemic unfolded, and COVID-related deaths surged in the sector, my Office was inundated with 269 complaints and inquiries. In an exceptional move, Canadian Armed Forces personnel were deployed to assist several Ontario long-term care homes that were experiencing crisis. In May 2020, it was reported that Armed Forces personnel had witnessed shocking living conditions in these homes.
6 Given the grave situation evident in the long-term care sector, on June 1, 2020, I initiated an investigation on my own motion into the Ministries of Health and Long-Term Care’s oversight of the sector during the pandemic. At the time, I announced that my investigation would focus on how the two ministries ensured the safety of long-term care residents and staff. Although my Office has broad investigative authority over ministries and the Patient Ombudsman, my authority does not extend to individual long-term care homes, their staff, or public health units.
7 As the pandemic continued to rage through the province, other bodies, including the Long-Term Care COVID‑19 Commission and the Auditor General, undertook their own comprehensive investigations and reviews. After considering the areas that had already been thoroughly explored, I decided that my investigation would provide the greatest value by concentrating on the Ministry of Long-Term Care’s inspections-related activity during the initial stages of the pandemic, and improvements that have been made since then. We focused on identifying further systemic changes and improvements that are necessary to ensure Ontario's long-term care sector is prepared for the next pandemic or similar health crisis.
8 Ombudsman staff sifted through more than 1.2 million documents and conducted 91 interviews for this investigation. What we uncovered was an oversight system that was strained before the pandemic, and proved to be wholly incapable and unprepared to handle the additional stresses posed by COVID-19. When the pandemic hit, the Ministry’s oversight mechanisms largely collapsed, with one Ministry employee describing it as “a complete system breakdown.”
9 During the critical initial weeks of the first wave, the Ministry’s Inspections Branch, which is responsible for receiving and inspecting complaints about long-term care homes, simply stopped conducting on-site inspections. For a seven-week period from mid-March to early May 2020, there was no independent on-site verification of the conditions in long-term care homes. The Inspections Branch did not clearly communicate its decision to stop on-site inspections to other areas of the government, long-term care homes, complainants or the public. Few knew that this oversight mechanism had fallen apart. In one area of the province, no on-site inspections occurred for three straight months.
10 Inspections stopped because the Ministry had no plan for inspectors to safely continue their work during a pandemic. The Branch did not have a supply of personal protective equipment, and inspectors were not trained on infection prevention and control. Once inspections resumed, and for much of the first wave, only inspectors who volunteered were sent to homes experiencing COVID outbreaks. Consequently, some areas of the province had as few as three or four inspectors to conduct on-site work, when there would normally be 20 to 25.
11 Rather than conducting inspections, the inspectors – who would typically be responsible for enforcing compliance with long-term care legislation – were tasked with “supporting and monitoring” long-term care homes through periodic telephone calls. Some homes refused to participate in these calls. At an already chaotic time, this switch to a new role and approach was confusing for long-term care homes and inspectors alike. In many cases, it also duplicated a function undertaken by other organizations.
12 The Inspections Branch was quickly overwhelmed by an unprecedented volume of complaints and questions from concerned families and caregivers. The Ministry did not adequately assess these complaints and conduct inspections when necessary. Instead, it primarily relied on inspectors to convey “key messages” over the phone and rebranded its complaints line as the “Family Support and Action Line,” resulting in confusion and undermining the compliance function of the Branch.
13 The Ministry put little thought into how its standard triage risk system would assess COVID-related complaints, resulting in a failure to categorize serious allegations as “high-risk.” It also took a narrow approach to its mandate and we discovered that extremely serious COVID-related issues – such as infection prevention and control or personal protective equipment usage – were not inspected in a timely manner, or at all.
14 In one case we reviewed, Peter[2] complained to the Ministry four times between April 6 and May 5, 2020, about disturbing conditions in his mother’s long-term care home. None of his concerns were inspected until October 2020, many months after his mother had already died from COVID. In total, 53 residents died at that same long-term care home during the first wave.
15 In another case, Gemma complained to the Ministry in April 2020 that her parents’ long-term care home was “severely short” on personal support workers. Gemma said residents were not being fed, cleaned or given their medications. One of Gemma’s parents had died of COVID, and the other was sick with the virus. A Ministry inspector "reassured” Gemma over the phone and then closed the file without taking any action. Thirty-three residents died at that long-term care home during the first wave. It’s impossible to know what might have happened if the Ministry inspectors had diligently followed up on complaints like Peter’s and Gemma’s when they were received.
16 In addition to its complaint-based inspections, the Inspections Branch conducts inspections in response to critical incident reports received directly from long-term care homes. Long-term care homes are required by law to report “critical incidents”, which are defined by legislation and include outbreaks of a disease such as COVID-19. Before the pandemic, the Ministry rarely did anything with critical incident reports about disease outbreaks. When the pandemic struck, many homes facing COVID-19 outbreaks did not report them as required and the Inspections Branch largely ignored their failure to make these reports. The Inspections Branch also did little – often nothing – when homes did file reports about COVID-19 outbreaks. By failing to follow up on these critical incident reports, as well as with the homes that failed to file them, the Ministry lost a valuable opportunity to inspect and intervene in homes facing outbreaks before conditions further deteriorated.
17 Our investigation also found that the Ministry took limited steps to enforce compliance with legislative requirements during the first wave of the pandemic. The Ministry’s Inspections Branch has authority to impose a range of enforcement actions or “penalties” when inspectors find a home in contravention of the law. In many of the first-wave situations we reviewed, the Branch chose to take only minor enforcement action, even when faced with significant and repeated non-compliance that put residents at risk.
18 We saw many examples where inspectors used their considerable discretion to lower the default enforcement action that would otherwise apply, even in very serious situations and with little to no explanation. One of the most severe responses available to the Ministry – a mandatory management order where the Ministry must approve a new operator for a home – was rarely considered, and there were no clear criteria guiding its use. In many cases, homes were instead permitted to enter into voluntary management contracts, which do not allow for the same level of Ministry control or oversight.
19 Even in situations where the Branch took enforcement action and required homes to comply with the legislation, homes were generally given many months to fix serious issues related to resident care and safety. We reviewed one instance where an inspector found that a long-term care home was not complying with legislated infection prevention and control requirements. The inspector determined that this was causing “immediate harm” to residents, and that the issue was “widespread” in the home – the highest categories of “severity” and “scope” associated with legislative contraventions. The inspector also noted that the home had a recent history of previous non-compliance on the same issue. The Ministry’s own internal procedures directed that in such circumstances, it should revoke the home’s licence and put an interim manager in place as the home is wound down. Instead of taking these actions, the Ministry issued a compliance order, which is a lower-level enforcement action, and gave the home three months to comply.
20 To foster transparency and accountability, the Ministry’s enforcement actions and inspection results are documented in public inspection reports. However, for more than two months during the first wave, the Inspections Branch stopped issuing any inspection reports, even for completed inspections that pre-dated the pandemic. Even when reports were released, we observed that they were often unduly lengthy, dense with acronyms, and poorly organized. Key information of interest was buried in different sections of the reports, making it difficult to navigate. In addition, the Ministry often combined totally separate complaints into one report. All of these practices made it very difficult for the public to identify whether a home had complied with orders made following an inspection.
21 Some will say that this is simply a snapshot in time, and that vast improvements have been made since then. To be sure, since the pandemic’s first wave, and as a result of recommendations made by other bodies, there have been some changes to the Ministry of Long-Term Care’s practices and to the legislation governing long-term care homes. In April 2022, the Fixing Long-Term Care Act came into force. It provides for new enforcement options. A new “investigations unit” is under development, which will focus on prosecuting the most serious contraventions. The legislation also requires long-term care homes to be better prepared for future pandemics, with numerous new requirements related to infection prevention and control practices, training, visitation policies, emergency planning, and staffing.
22 Beyond these legislative changes, the Inspections Branch has also taken steps to better prepare itself to respond to a future pandemic. It has also committed to conducting periodic, proactive inspections at each long-term care home, and the government has increased its staffing levels to handle this increased workload.
23 Nevertheless, it is crucial that the Ministry fully understand and learn from the failure of the Inspections Branch to adequately and quickly respond to the emergency that arose in the long-term care sector in March 2020. Nearly 80,000 vulnerable long-term care residents rely on the Ministry of Long-Term Care’s oversight to ensure their homes are safe and secure. Tragically, it was unprepared and unable to ensure the safety of long-term care residents and staff during the pandemic’s first wave. It is my opinion that this was unreasonable, unjust, and wrong under sections 21(1)(b) and (d) of the Ombudsman Act.[3]
24 While the Ministry has already taken some steps to better prepare itself for the next emergency, the Inspections Branch must be ready to fulfill its mandate, no matter the circumstances. I have made 76 recommendations in this report. Of these, 72 are directed to the Ministry, two call on the Government of Ontario to support the Ministry in carrying out its legislative responsibilities, and two urge the Ministry and Government to work together to ensure the Ministry has sufficient inspectors and staff going forward. My report does not focus on or make recommendations to the Ministry of Health, which has been the subject of other reviews that resulted in numerous findings and recommendations.
25 Experts warn us that there will eventually be another pandemic. Evidence is building that climate change, combined with our ever-greater encroachment into wildlife habitat, is fuelling the risk of viruses spilling from animals into humans. “There will be another pandemic. Like death and taxes, it’s an absolute certainty,” says Dr. Allison McGeer, an infectious disease specialist and professor of laboratory medicine and pathobiology at the University of Toronto’s Dalla Lana School of Public Health.[4]
26 We likely don’t have years to wait until the next pandemic. As Professor Jacob Lemieux from Harvard Medical School has noted, “we are seeing pandemics emerge frequently, not once in a lifetime, but in fact every few years, and we need to start preparing.”[5] Policy makers must demonstrate leadership and unity to combat future public health threats.The people of Ontario should be able to count on their public services to learn lessons from our experience with COVID-19 and be adequately prepared for the next threat to our collective health.
27 I am hopeful that these evidence-based recommendations, aimed at building on changes already in progress and enhancing pandemic preparedness in the inspection regime for long term care homes, will ensure that the Ministry is able to effectively meet its vital oversight responsibility during the next health crisis.
A Tragedy of Epidemic Proportions
28 The effects of the multi-year COVID-19 pandemic on Ontario’s long-term care sector have been severe and deadly. Although long-term care residents represent a tiny fraction of Ontario’s population, they account for nearly one-third of the province’s COVID death toll.
29 The first wave of the virus had a devastating impact on the long-term care sector, arriving at a time before vaccines were available and when personal protective equipment supplies and infection prevention and control expertise were hard to find. Some 1,937 COVID-related deaths occurred in the sector during the first wave, from January 15, 2020 to August 2, 2020. The vast majority of the other COVID-related deaths in the sector arose during the pandemic’s longer second wave, from August 2020 until February 2021. The availability of vaccines beginning in December 2020 was credited with substantially reducing the incidence of serious illness and death in long-term care residents thereafter.[6]
30 The impact of the pandemic was inconsistent across individual long-term care homes. For example, the 233-bed Orchard Villa home in Pickering experienced 70 resident deaths due to COVID. Meanwhile, other homes experienced no large outbreaks and few deaths.
31 The arrival of COVID-19 in Ontario evoked an unprecedented response. At times, precautionary measures in the long-term care sector came at the price of the individual rights of residents, including to receive visitors.[7] For instance, on March 13, 2020, Ontario’s Chief Medical Officer of Health strongly recommended that all long-term care homes allow visitors only for residents who were very ill or nearing the end of their life.[8] A few weeks later, the Chief Medical Officer required that long-term care homes “be closed for visitors, except for essential visitors.”[9] Family and volunteers who provided care services required to maintain residents’ health were later described as “essential visitors.” This restriction on visits remained in place for a long time, and deprived many residents of a significant source of family support. As one resident told us:
“…my world change[d]. I became a non-citizen…without the ability to make choices and decisions on how I live my life.”
32 Compounding the isolation were restrictions on residents’ movements within the homes. Many were mostly confined to their rooms, further reducing their opportunities for human contact. One resident told us it felt like being “in jail.” She added:
“I think the worst thing – and I’m sure I speak for a lot of residents – was the fact that we missed our families so much. That to me was the worst thing of the whole pandemic… I missed my family.”
33 The mandatory restrictions were also acutely felt by families and friends of residents. Prior to the pandemic, they could not only visit with residents to provide care and support, but observe their living conditions firsthand and report any concerns about their care to management and the Ministry. When they were shut out of the homes, an important connection with residents was lost, as well as a valuable source of information about the adequacy of care.
34 Many homes also suffered from staffing issues during the pandemic, and the absence of support from family and other caregivers increased the difficulties caused by those shortages. We heard of multiple homes during the first wave where more than 80% of staff tested positive for the virus at the same time, leaving most unable to work. We heard many examples of the impact this had on residents. In April 2020, according to a Ministry of Long-Term Care inspector, a staff person at the Orchard Villa home in Pickering called the Ministry to report that “…there is no staff to feed and care for residents, and that living conditions are like hell.” Ministry inspectors did not enter homes during the peak of the first wave, so there was little external oversight as homes struggled to meet residents’ basic needs.
35 The first wave also severely affected long-term care staff on the front lines in individual homes. Canadian Armed Forces personnel who were called in to help described the workers they supported at one home as overworked and burned out, and noted many had “not seen their families for weeks.”
36 Officials from Canadian Union of Public Employees Ontario told us many of their Ontario members working in the homes were physically and emotionally exhausted during the first wave. They said some were given the task of putting residents’ bodies into body bags, far from their typical duties, and that these staff would feel the psychological impact “for years to come.” A senior official at the Ontario Personal Support Workers’ Association had similar comments, comparing long-term care homes during the first wave to a “battlefield.” Although my Office does not oversee the living or working conditions in individual long-term care homes, the horrendous conditions experienced by many long-term care residents and workers provides important context for assessing the role played by the Ministry of Long-Term Care’s Inspections Branch during the first wave.
Investigation Scope and Process
37 In June 2020, I informed the Ministry of Health and the Ministry of Long-Term Care that my Office would investigate the adequacy of their oversight of the long-term care sector during the coronavirus (COVID-19) pandemic. The investigation was launched on my own initiative and was to examine how the two ministries ensured the safety of long-term care residents and staff. I made this decision after the publication of a letter[10] by the Canadian Armed Forces (CAF) personnel that provided disturbing details about the conditions in long-term care homes that had received CAF assistance. I was also disturbed by the growing number of COVID outbreaks and COVID-related deaths in long-term care homes across the province, as well as an increase in complaints to my Office.
38 Although other reviews were underway or had been announced, I was confident that my Office’s privileged relationship with Ontarians and the singular perspective we are afforded by hearing directly from people and working to resolve their individual complaints would enable us to make a unique and valuable contribution to finding solutions.
39 A previous investigation by this Office in 2008 regarding the province’s oversight of the long-term care sector identified several issues, which were set out in a letter tabled with the Ontario Legislature in November 2010.[11] These issues were considered by the then-Ministry of Health and Long-Term Care as it made numerous legislative and operational changes to modernize the sector.[12]
A challenging investigation
40 When I announced this investigation in June 2020, few could have known the ways in which COVID would affect day-to-day life over the coming years. As those impacts became clearer, and as other organizations undertook their own investigations and reviews, I decided that my investigation would produce the greatest impact by focusing on the Ministry of Long-Term Care’s inspections-related activity during the initial stages of the pandemic, with a view to recommending improvements that will strengthen oversight for the future and ensure that the Ministry and Ontario’s long-term care homes are better prepared for the next pandemic. Other matters related to COVID in the long-term care sector, such as pandemic planning, responses to subsequent waves of infection, licensing of homes, and steps taken by the Ministry of Health, have been investigated and reported on by other organizations.[13]
41 The Special Ombudsman Response Team (SORT) led this investigation, supported by other staff from our Generalist Early Resolution and Investigations teams, as well as Legal Services staff.
42 In response to our requests, we received more than 1.2 million documents – mostly emails and their attachments. We conducted 91 interviews with staff from the ministries of Long-term Care and Health, other government officials, long-term care home administrators, and other relevant stakeholders. We also obtained information from the Canadian Armed Forces. In addition, we met virtually with officials from the Ministry of Long-Term Care and the Ministry of Health on several occasions to obtain information about their operations, and to receive updates on changes to legislation, policies and other relevant initiatives.
43 It was difficult to conduct such a large and complex investigation during the pandemic. This was one of the first Ombudsman investigations conducted while staff worked remotely, and it was necessary to put new information technology infrastructure in place to allow staff to effectively and confidentially carry out their work. While remote work is now second nature to many, in June 2020 it was a major departure from our typical investigative approach.
44 Our investigation was also affected by the workload of staff at the ministries we were investigating. Understandably, many were preoccupied with responding to the ongoing impact of the pandemic, especially as it became clear that the second wave of the pandemic would be even more devastating than the first. We also heard that requests relating to other reviews and investigations, including those of the Auditor General, Long-term Care COVID-19 Commission, and Patient Ombudsman, hampered staff’s capacity to respond to our requests. We also struggled to interview several key individuals due to leaves of absence, retirements, other urgent priorities, and numerous personnel changes.
45 Cognizant of the challenges facing public sector officials, we worked collaboratively to determine how and when documents would be provided and interviews scheduled. For example, we allowed the ministries to provide documentation in instalments – a departure from our usual process. We also allowed interviewees to reschedule their time with us if they were urgently needed elsewhere.
46 This approach, unfortunately, dramatically affected the timeliness of the information we received. For example, it took Ministry officials more than three months to answer our request for basic information about inspectors, which we needed in order to decide which inspectors to interview. When we finally received a response, it was too late to be useful in the investigation and did not offer us the details we had requested. It also took more than seven months for officials to begin sending us copies of certain Ministry inspection files that were key to our investigation.
47 Most concerning, the Ministry did not provide copies of all relevant emails and email attachments for more than a year. During this lengthy delay, we worked diligently with the Ministry and a third-party vendor it hired to provide detailed information about our request. When concerns were raised about the volume of emails that would be produced, we narrowed the date range and scope of our request. We were told that this would yield about 67,000 emails – a large, but manageable number. What we ultimately received was very different – a mass of over 1 million emails with no organization by subject-matter. More than 300,000 documents were unsearchable PDFs, provided without context or other form of organization. My Office’s Information Technology team was able to develop some solutions, but given the sheer volume of information, it was not possible for investigators to read every email and document. Instead, we relied on filters, sorting, and targeted searches to select documents most likely to be relevant to our investigation.
48 These delays, and the volume of information produced, impacted our ability to conduct interviews in a timely manner, since, as a best practice, we try to review the key documents relevant to witnesses before we speak with them.
49 It was also difficult to confirm whether the Ministry provided us with all the relevant information we had requested. The Ministry withheld or redacted more than 38,000 documents because they contained information that the Ministry said did not need to be disclosed – e.g., due to solicitor-client privilege. It is common for organizations to assert this type of privilege during Ombudsman investigations, but it usually does not apply to a large number of documents, and we normally receive a detailed explanation as to why each document is being withheld. In this case, we only received a spreadsheet listing basic details about the 38,000 records, and there was little explanation for why each withheld document was privileged. When we asked a senior Ministry official to clarify how the government determined which records were subject to privilege, we were told that they relied on specific software to do an initial search, with Ministry lawyers “auditing” the search results. It was impossible for our staff to determine if documents had been properly withheld.
50 Despite these obstacles, we appreciate the co-operation we received from the Ministries and acknowledge the serious challenges they faced in trying to respond to the pandemic itself, our investigation, and several other reviews and investigations.
51 This investigation required a tremendous amount of planning and preparation. The investigative process – particularly interviewing witnesses and obtaining documentary evidence – was hampered considerably by the state of public health, staffing levels and having to conduct much of the work virtually. Nonetheless, it was imperative that we conduct a thorough and rigorous investigation that took account of the situation from a variety of perspectives.
52 Moreover, our Office was not at its full staffing complement during this investigation, which also affected timelines. Two significant expansions of the Ombudsman’s mandate (in 2016 and 2019) not only greatly increased the scope of our jurisdiction but also resulted in higher caseloads. Although we have added staff and continue to do so, during the period of this investigation our human resources unit lacked the capacity to get us to a full staffing complement and optimize our operations.
Cases received
53 This investigation was launched on my own motion. However, my Office has broad authority to review complaints about the administrative conduct of the Ministry of Long-Term Care, as well as the Patient Ombudsman, who has a mandate to directly review complaints about long-term care homes and other health services. My Office’s mandate does not include complaints about individual long-term care homes, their staff, or public health units.
54 We received 269 cases (complaints and inquiries) related to the issues under investigation. Most of these were received at the height of the pandemic’s first wave and related to concerns about the government’s handling of the pandemic in the long-term care sector. Many came from family members of long-term care residents and raised general concerns about the government’s planning and early response, as well as specific issues related to personal protective equipment, COVID testing, infection prevention and control, and restrictions on visitors. We also received a significant volume of cases from long-term care home staff, family councils and other stakeholders. Some of these were about how the Ministry communicated important pandemic-related information to Francophones; these cases were dealt with by my Office’s French Language Services Unit.
55 Many of the cases we received related to issues in individual long-term care homes, and our Early Resolution Officers referred them to the Ministry of Long-Term Care’s Inspections Branch, the Patient Ombudsman or to other resources, such as the Advocacy Centre for the Elderly.[14] Many others raised concerns about the Ministry’s inspection and complaints process, including issues such as delayed responses, inadequate investigations of complaints, poor communication, and disagreement with the Ministry’s enforcement actions or lack thereof. Ombudsman staff worked to resolve these individual issues, while the evidence they gathered helped guide our investigation.
56 We received very few complaints directly from long-term care residents, and while it is impossible to know exactly why, there are many potential reasons. Most residents require extensive help with daily activities, including the use of a telephone or computer. Many experience some form of cognitive impairment or neurological disease that may make it difficult or impossible to contact my Office. To assist in understanding the perspective of residents in such situations, our investigators spoke with long-term care residents and other representatives involved with the Ontario Association of Residents’ Councils and Family Councils Ontario.
57 In addition to receiving and resolving individual complaints, my Office’s French Language Services Unit also worked to ensure that the needs and interests of Francophones were considered by the Long-Term Care COVID-19 Commission. Following this input, the Commission invited Francophones to appear before it to assist in analyzing the specific issues affecting them and identifying solutions. In its report, the Commission recognized that Francophone long-term care residents must receive culturally and linguistically appropriate care and services, and made two recommendations related to French language services.[15]
Long-term Care in Ontario
58 There are more than 600 long-term care homes in Ontario, comprising nearly 80,000 resident beds. These homes are places where adults can receive help with most or all daily activities and access to 24-hour nursing and personal care.[16] Long-term care residents are some of the most vulnerable people in Ontario. The vast majority of residents need extensive help with tasks such as getting out of bed, eating, or toileting, and experience some form of cognitive impairment or neurological disease.
59 The long-term care home sector is large, employing more than 100,000 people in the province. Around 60% are personal support workers, who help residents with bathing, dressing, eating, and moving around the home. Another 25% are registered nurses or registered practical nurses.[17] Doctors and other medical professionals also provide care to residents.
60 Through most of the pandemic, the Long-Term Care Homes Act, 2007 and Ontario Regulation 79/10 governed the provision of long-term care.[18] In April 2022, these laws were repealed and new legislation, the Fixing Long-Term Care Act, 2021 came into force.[19] Both Acts establish a similar structure for the provision of long-term care services and Ministry oversight.
Ministry of Long-Term Care
61 The Ministry of Long-Term Care is responsible for licensing long-term care homes, receiving complaints, conducting compliance inspections, and taking enforcement action if a home is not complying with legal requirements.
62 As of March 2020, the Ministry’s Operations Division handled inspections, enforcement and licensing. Within this division, the Inspections Branch is responsible for inspecting homes to ensure they are complying with legislation and any Ministry directives. If a long-term care home is not in compliance, the Branch decides what enforcement action to take.
63 Long-term care homes are owned by a range of entities, including municipalities, for-profit companies, and non-profit organizations. Each owner and long-term care home must be licensed by the Ministry of Long-Term Care.[20] The Ministry has broad authority when licensing homes and can add conditions to a home’s licence, amend a licence, and revoke a licence completely, if necessary. At the start of the pandemic, the Licensing, Policy and Development Branch was responsible for this function, although in June 2020 it shifted to the Long-Term Care Capital Development division.
Other sources of oversight
64 In addition to the Ministry of Long-Term Care, other organizations oversee long-term care homes, including the Ministry of Health, local public health units, and the Patient Ombudsman.
Ministry of Health
65 Among many other mandates, the Ministry of Health is responsible for the planning and co-ordination of emergency response for the whole health system, including the long-term care sector. This role is set out and guided by the Emergency Management and Civil Protection Act, and Ontario Regulation 380/04.[21] While this legislation gives this responsibility to the Ministry of Health alone, we were told that in practice it carries out its responsibility in co-ordination with the Ministry of Long-Term Care.
66 The Office of the Chief Medical Officer of Health is part of the Ministry of Health, and the Health Services Emergency Management Branch reports to that office. This branch is responsible for the policy, programming, planning and co-ordination work for emergencies across the health care sector, including in long-term care homes.
Patient Ombudsman
67 The Patient Ombudsman is responsible for taking complaints about the care and health care experience of residents in long-term care homes, patients in hospitals, and individuals receiving services from Home and Community Care Support Services.[22] Like our Office, it is considered the “recourse of last resort.” The Patient Ombudsman attempts to resolve long-term care home complaints through mediation and negotiation, or through investigation if necessary.[23] It has released three “special reports” during the pandemic on complaints about long-term care homes.[24]
Local public health units
68 Ontario is divided into 34 geographic areas called public health units.[25] Each is led by a local medical officer of health who reports to the local board of health, and is responsible for taking action to safeguard the public’s health at a local level. Local medical officers of health and their public health units assist in identifying and managing outbreaks of disease in long-term care homes and provide proactive outreach and education. Public health units can also inspect infection prevention and control practices in long-term care homes, although most do not do this proactively.
69 If warranted, local medical officers can issue orders to long-term care homes under the Health Protection and Promotion Act, requiring them to take (or refrain from taking) certain actions. During the first wave of the pandemic, several public health units used this power to impose conditions on long-term care homes that were struggling to cope with outbreaks.
70 The Health Protection and Promotion Act requires long-term care homes to report cases of certain diseases to their local public health unit as soon as possible, and since January 22, 2020, COVID has been a reportable disease.[26] The Ministry of Health created a guide called the Institutional/Facility Outbreak Management Protocol, which sets out what public health units should do when responding to reported outbreaks of disease in certain settings, including long-term care homes.[27] The guide specifies that public health units “assist” facilities, while the homes themselves retain responsibility for managing outbreaks.[28]
71 In the first wave of COVID, there was little guidance for public health units about what role they were supposed to play during a widespread pandemic, especially in the context of long-term care homes. The government’s 2013 Ontario Health Plan for an Influenza Pandemic provided some general guidance for what the units would do, such as collecting and analyzing local data, leading local immunization efforts, and developing and issuing orders.[29] However, there were no specific sections related to public health units in the context of long-term care, and we heard that different public health units took differing approaches during the first wave of the pandemic.
72 My Office has no authority to review complaints about public health units, and in 2020-21, we had to turn away 87 cases about them. This included issues related to COVID testing, contact tracing, mask and social distancing guidelines, local orders, and access to vaccines. I flagged this serious issue in my 2020-21 Annual Report, noting that:
Public health units have been central to Ontarians’ experience of the pandemic, responsible for everything from playground closures to mask mandates to vaccination operations. Their work is crucially important and their decisions collectively affect millions. And yet they operate without oversight: They are exempt from the jurisdiction of my Office, and that of the Ministry of Health’s Patient Ombudsman.[30]
73 At that time, I encouraged the province to implement independent oversight of public health units. In 2021-2022, we received another 137 cases about public health units, which we were unable to address.[31]
A Focus of Inquiry
74 Several oversight bodies with varying mandates have conducted reviews and made recommendations related to the long-term care sector and the province’s response to the COVID-19 pandemic. Substantial expertise, time and money went into the important work of these other organizations, and my own investigation is meant to build upon, not duplicate, their findings and recommendations.
Gillese Inquiry
75 Between 2007 and 2016, registered nurse Elizabeth Wettlaufer intentionally gave insulin overdoses to a series of long-term care home residents. Her actions killed eight people, and seriously harmed at least six others. She later confessed, resulting in her prosecution and conviction.[32]
76 After the trial, the Ontario government asked the Honourable Justice Gillese to lead a public inquiry into the safety and security of residents in Ontario’s long-term care homes. The inquiry was held between 2017 and 2019, and Justice Gillese’s final report was released on July 31, 2019.[33]
77 The report made three central findings: That no one would have discovered what Elizabeth Wettlaufer did had she not confessed; that the events were the result of systemic vulnerabilities in the long-term care system; and that the long-term care sector is “strained but not broken,” with long-term care homes under pressure because they have limited resources.[34]
78 Among the report’s many findings and recommendations was a call for the then-Ministry of Health and Long-Term Care to create a dedicated unit to support long-term care homes in achieving compliance with the law.[35] It also made a series of recommendations around the reporting of serious incidents to the Ministry, and about how the Ministry should inspect the highest-risk issues. Specifically, it called on the Ministry to tweak its performance assessment methodology to give more weight to “high-risk” issues, which should be inspected as quickly as possible to mitigate the risk of harm to residents.[36] It asked the Ministry to use performance data to help it determine how quickly to inspect issues, and to act when the data shows a home is struggling to provide a safe and secure environment.[37] It further asked the Ministry to educate the public about which incidents must be reported.[38]
79 The Gillese report also recommended the Ministry carry out a study to determine adequate staffing levels for homes.[39] This study was done largely during the pandemic’s first wave and was tabled in July 2020. The resulting report recommended that each resident receive a minimum daily average of four hours of direct care and called on the government to provide additional funding for homes to achieve that goal.[40] This latter report recommended that the government create guidelines on staffing ratios and mix and called for better recognition for the role of personal support workers and greater use of nurse practitioners. It also made numerous recommendations about working conditions for long-term care staff. Some of the recommendations made by this study have been incorporated into the Fixing Long-Term Care Act, 2021, which came into force in April 2022.
Independent Long-Term Care COVID-19 Commission
80 The largest and most comprehensive review of COVID-19 in the long-term care sector was conducted by the Independent Long-Term Care COVID-19 Commission. The Commission was announced in May 2020 and formed on July 29 that year, with a mandate to investigate how and why COVID-19 spread in long-term care homes, what was done to prevent the spread, and the impact of key elements of the existing system on the spread.[41] The Commission issued interim reports in October and December 2020, and its final report was published in April 2021.
81 The October 2020 interim report provided the government with early recommendations that it could implement immediately as a growing second wave of the virus quickly overtook long-term care homes.[42] Among other things, it called for improved staffing and asked the government to help the homes build better relationships with local hospitals and public health units.[43] It suggested that every home have a dedicated infection prevention and control lead, and that Ministry inspectors should ensure that homes were following infection, prevention and control procedures properly.[44]
82 The Commission released its second interim report in December 2020 as the pandemic continued to worsen. Among its recommendations were a requirement that homes report and publicly post more data, including staffing levels and supplies of personal protective equipment.[45] It also called on the Ministry of Long-Term Care to restart its proactive resident quality inspections (RQIs) at all homes, and include a review of infection prevention and control practices as part of all reactive inspections. To operationalize these inspections, it recommended that the government give the Ministry enough money to hire and train inspectors to carry out an RQI at every home every year. It further recommended that the Ministry respond faster when it issues orders for IPAC and “plan of care” issues.[46] Additionally, it urged the Ministry of Long-Term Care, the Ministry of Labour, Training and Skills Development and public health units to co-ordinate their inspections and share information.[47]
83 The Commission published its final report in April 2021. At over 300 pages, it provided a detailed review of the state of the long-term care sector before and during the pandemic (to that point), and the many factors that affected the ability of homes to keep residents safe from COVID. It made 85 recommendations.[48]
84 Quoting extensively from the experiences of residents, family members, caregivers and long-term care home staff, the Commission said each group “suffered terribly” during the pandemic. Residents were “neglected, scared, alone and cut off from those they love and depend on.” Meanwhile, the long-term care home staff who were able to keep working watched their residents die – and then sometimes had to prepare the bodies after death, leaving many traumatized.[49]
85 The Commission made strong comments on the government’s lack of planning for a pandemic like COVID-19. It noted that for years, the province had implemented important recommendations from previous reports to prepare for a future pandemic – including several studies arising from the 2003 Severe Acute Respiratory Syndrome (SARS) outbreak.[50] But over time, the province “lost the will to make pandemic preparedness a priority,” the Commission said, even though it was foreseeable and inevitable that a deadly pathogen would someday sweep the world.[51] According to the Commission’s report, when COVID emerged, the province didn’t have an up-to-date pandemic plan. The existing plan focused on influenza, had not been updated since 2013, and contained no specific guidance for the long-term care sector. Instead, the province had invested years of work in a new “ready and resilient health system” plan, which was not ready when COVID arrived.[52] The Commission said planning for a pandemic must be a constant priority, and called on the government to finalize its plan, make it public, and include specific guidance for long-term care. It also stressed that every long-term care home should have its own pandemic plan.[53]
86 The Commission’s report also discussed the adequacy of the province’s emergency supplies at length. It notes that in 2017, the province discovered that most of its stockpile of emergency health supplies had expired after being amassed in the wake of the SARS outbreak. The province ordered the destruction of 90% of the stockpile and spent three years deliberating on whether and how to replace it.[54] In addition, there was no requirement for long-term care homes to have a specific supply of personal protective equipment. By the time COVID arrived, the province’s supply of usable equipment had been significantly depleted and there was no way of knowing the state of supplies at individual long-term care homes. The Commission recommended that the government enact legislation regarding the provincial stockpile, and put the Chief Medical Officer of Health in charge of it. It also called on the government to actively manage its emergency supplies and ensure long-term care homes have priority access.[55]
87 The Commission also found that uncertainty around roles and responsibilities made the situation even more precarious. When the pandemic began, a large number of organizations were merging into the new Ontario Health agency, leaving some key responsibilities unfilled or unclear. One agency that should have been central to the pandemic response – Public Health Ontario – was underfunded and out of the loop. Further, the recent creation of a separate Ministry of Long-Term Care meant that its responsibilities hadn’t been fully delineated, leaving the new ministry “fighting to be heard.”[56]
88 The Commission’s report also found that when the virus arrived, the government didn’t have a command structure ready and was making up its response as it went along. It said officials were confused about who was doing what, and who was actually in charge. Key public health decisions were not made by experts and there was poor communication between the different “tables” tasked with pandemic response. Notably, the government didn’t create a response table for long-term care until late-April 2020.[57]
89 With respect to the long-term care sector, the Commission found that homes were highly vulnerable when the pandemic began because successive governments had failed to tackle longstanding problems, including chronic underfunding, severe staff shortages, outdated infrastructure, and inadequate oversight. To compound these issues, the homes were poorly connected to the rest of the health system. After SARS, long-term care homes lost their links with hospitals because they were supposed to get their own infection prevention and control (IPAC) experts. But the role of internal IPAC lead within homes often fell to an “otherwise busy nurse” who was not primarily devoted to the task.[58] The Commission recommended that the government require homes to have their own full-time IPAC practitioners, better training around IPAC, and formal links with the rest of the health system.[59]
90 The Commission wrote at length about the impact of inadequate staffing in homes. It found existing staffing levels were insufficient, and constant shortages, excessive workloads, high turnover rates, and heavy reliance on part-time workers are common in the sector. Specific to COVID, the Commission observed that the government was too slow to limit long-term care home staff to working at one location to prevent the spread of disease between homes, and the government had no plan to replace workers who stayed away when outbreaks struck, causing “many residents to suffer from malnutrition and dehydration, sometimes with fatal consequences.”[60] The Commission called on the government to address staffing shortages, and to build a bigger long-term care workforce with the necessary mix of skills.[61]
91 Regarding inspections, the Commission found that the “almost total elimination” of the proactive resident quality inspections (RQIs) before the pandemic “left the Ministry of Long-Term Care with a very limited picture of the state of long-term care homes, and virtually no idea of a home’s IPAC and emergency preparedness when the pandemic began.”[62] It described the Inspections Branch as “missing from action and invisible” during the pandemic, lacking both direction and inspector capacity during the first wave.[63] The Commission recommended the Ministry conduct more timely inspections of infection prevention and control and carry out a proactive inspection of each home annually. It also called on the government to provide the Ministry enough funding for the necessary inspectors.[64]
92 The Commission specifically commented on the Ministry’s lack of enforcement when homes failed to comply with the law. It noted the Ministry of Long-Term Care rarely used Director’s Orders and fines, and instead took low-level actions for most situations of non-compliance. It said the absence of strong action likely explained the lack of urgency among long-term care operators to comply with the law, and called on the Ministry to take “proportionate and escalating consequences” for non-compliance.[65]
93 Overall, the Commission found that the government “failed to prioritize long-term care before the disease had already gained a fatal foothold in homes.”[66] Its report noted the government did not heed the experiences of other jurisdictions, even though by mid-March 2020, many other jurisdictions had already seen high death rates in long-term care from COVID. Rather, it observed, the government continued to tell the public the risk posed by COVID was “low,” even after officials agreed in private that spread was inevitable.[67]
94 After the report’s release, the Minister of Long-Term Care committed to reviewing the final recommendations carefully in the government’s ongoing efforts to fix the systemic issues facing Ontario's long-term care sector. The Ministry has since implemented a number of the Commission’s recommendations. For instance, in late November 2021, it restarted proactive inspections, which are now called “proactive compliance inspections.”
Office of the Auditor General of Ontario
95 The Auditor General has also issued several reports regarding the province’s oversight of long-term care homes.
2015 special report and 2017 follow-up
96 In a 2015 special report regarding long-term care oversight, the Auditor General found that the then-Ministry of Health and Long-term Care was taking too long to inspect high-risk complaints and critical incidents in long-term care homes.[68] The report said this was because the Ministry had focused its resources on annual, proactive resident quality inspections, which caused a growing backlog for complaint and critical incident-driven inspections. It also found the Ministry was not appropriately prioritizing its proactive inspections according to the risk each home presented.[69]
97 With respect to the inspections it did conduct, the Auditor General noted that the Ministry gave homes inconsistent timelines to implement its orders, and then often failed to re-inspect homes within the timeframe it had selected. The timeliness and effectiveness of the Ministry’s inspections varied significantly across the province.[70] The 2015 report specifically called on the Ministry to take stronger action to address repeated non-compliance in certain long-term care homes.[71]
98 In 2017, the Auditor General released an update on this investigation, indicating the Ministry had only made patchy progress on the issues identified in 2015. This report said the Ministry had developed a shorter version of its comprehensive resident quality inspection (RQI), and would only conduct a full RQI at each low-risk home every three years, instead of annually. The Ministry was referring more cases of repeated non-compliance to the Director, and planned to introduce new enforcement measures through legislative change. However, the Auditor General found the Ministry still had a large backlog of complaints and critical incidents that needed inspection.[72]
Special COVID-19 audit
99 In response to the COVID-19 crisis, the Auditor General conducted a special audit into the province’s response and released her findings as six separate “chapters” through 2020 and 2021.[73] One of those chapters – Chapter Five: Pandemic Readiness and Response in Long-Term Care – specifically addressed the impact on the long-term care sector. It was released in April 2021 and covered the period from January 2020 to December 2020.[74]
100 The chapter identified three central issues that made it difficult for the government to respond to the needs of long-term care homes. First, it found that the province had taken insufficient action to implement the many observations and recommendations made after SARS to ensure Ontario was better prepared for “next time.” Second, the government generally hadn’t addressed systemic weaknesses in the delivery of long-term care. Third, the lack of integration between long-term care and the rest of the health care sector, compounded by an ongoing reorganization of the sector, left long-term care homes without access to infection prevention and control expertise at the start of the pandemic.[75]
101 The chapter also outlined a series of pre-existing concerns with the Ministry of Long-Term Care’s Inspections Branch that left homes more vulnerable to disease. It stated that the long-term care legislation wasn’t strong or specific enough to enable inspectors to check whether homes had good infection prevention and control programs, and the vast majority of the inspectors didn’t have enough IPAC knowledge to do so. It noted the Ministry had historically inspected very few outbreaks of disease in long-term care, and that after proactive inspections were discontinued, few IPAC issues were found during inspections. It also observed the Ministry’s decision to pause resident quality inspections was contrary to the Auditor General’s 2015 audit recommendations and compromised the Ministry’s oversight of homes.[76]
102 The Auditor General also identified many problems with the Ministry’s Inspections Branch once the pandemic arrived, including the Branch’s failure to conduct on-site inspections for an extended period. She noted that it mainly used low-level enforcement actions, even in the face of repeated non-compliance with the law.[77]
103 Another chapter of the Auditor General’s COVID-19 special report reviewed the government’s outbreak planning and decision-making for the health sector more broadly. It indicated the province hadn’t updated its pandemic plan since 2013 and found that those making key decisions were not public health experts, that Public Health Ontario had played a diminished role, and that the Chief Medical Officer of Health did not exercise his full authority. It stated that the government failed to follow the lessons from SARS, and that it characterized the risk of COVID as low despite the inevitability that it would spread. It also observed the province took too long to compel long-term care staff to wear masks and to prohibit long-term care staff from working across multiple sites.[78]
104 A further chapter, released in December 2021, reviewed the supply of personal protective equipment (PPE) in the province. The Auditor General noted that her office reported in 2017 that most PPE in the province’s stockpile had expired and the government was destroying it without replacing it. The chapter said the government’s efforts to centralize the PPE supply chain were not ready, and health care workers, including long-term care home staff, were not always properly protected with PPE.[79]
105 The other chapters of the Auditor General’s Special COVID-19 Report highlighted issues with testing, case management and contact tracing, expenditures and planning for non-health settings.[80]
Patient Ombudsman
106 The Patient Ombudsman has direct oversight of long-term care homes. On June 2, 2020, that office announced its first-ever systemic investigation, into the experiences of residents and caregivers in long-term care at the onset of the pandemic.[81] The Patient Ombudsman has issued three special reports setting out the types of complaints the office has received,[82] as well as the results of a survey of residents, family members and staff.[83]
107 The Patient Ombudsman’s first special report was released in October 2020 and summarized the most common complaints in long-term care during the first wave.[84] These included concerns about visitation restrictions and infection prevention and control, as well as communication issues. The report made some preliminary recommendations, including that every long-term care home should partner with an outside organization, such as a hospital, to obtain the necessary resources to respond to COVID outbreaks. The report also recommended all homes have a plan to manage significant staffing shortages, outbreaks and infection prevention and control matters. The Patient Ombudsman also urged the government to ensure “essential caregivers” could still visit and communicate with residents.
108 The Patient Ombudsman’s second special report was released in August 2021 and covered complaints from the second and third waves of COVID about long-term care, public hospitals and home and community care. The report offered an update on the most common long-term care complaints, and some examples of the stories his office heard from residents and caregivers. He recommended the government guarantee long-term care residents the right to receive visitors, and ensure that any restrictions on visits were necessary and risk-based. As well, he called for more supports for health care workers and said long-term care homes should have a plan in place to communicate significant policy changes that affect residents and caregivers.[85]
109 The Patient Ombudsman’s third special report was released in December 2021 and summarized the results of surveys of long-term care home residents, their loved ones and staff about their pandemic experiences. The report noted the effect of “chronic staffing shortages, as well as the impact of prolonged isolation and lack of stimulation on residents’ emotional health and well-being.”[86] It observed that many loved ones were still struggling to visit residents, and reiterated that balancing infection prevention and control measures with residents’ quality of life was a critical challenge.[87]
110 These reports by the Patient Ombudsman, the Auditor General, and the Independent Long-Term Care COVID-19 Commission made important contributions to understanding the impact of COVID-19 in Ontario and led to significant recommendations for improvements. Although my Office’s investigation focused on the same event, it did so from a unique perspective, shaped by our expertise in administrative fairness. We explored in great depth how the Ministry of Long-Term Care’s Inspections Branch responded to the crisis and how it addressed the serious concerns brought forth by long-term care home residents, their family members and other caregivers. In doing so, we were able to identify systemic issues that directly affected the adequacy and responsiveness of the Branch’s inspections and the remedial measures taken to address non-compliance by long-term care homes. The impact of systemic problems within the Branch was heightened during the pandemic’s first wave. However, many of the issues we discovered reflected pre-existing administrative flaws that transcended the pandemic. In addition, our investigation revealed significant new evidence about how the Ministry of Long-term Care’s Inspections Branch responded to the challenges of the pandemic’s first-wave, and it is important that this information be part of the public record and discourse.
The Inspections That Never Were
111 As other reports and investigations relating to COVID-19 have demonstrated, the long-term care sector has faced chronic challenges, which the pandemic magnified intensely. One of the Ministry of Long-Term Care’s greatest failings during the first COVID wave was its inability to mobilize its inspectors as successive long-term care homes succumbed to outbreaks. For an extended period, the Ministry’s oversight of the sector was essentially non-existent, as its primary tool for assessing the living conditions within Ontario’s long-term care homes – on-site inspections – was shelved.
The inspection landscape as COVID-19 arrived
112 The Ministry of Long-Term Care relies on inspections to determine whether a long-term care home is complying with its legislative obligations. Prior to the pandemic, the Inspections Branch typically conducted about 3,000 inspections annually in accordance with its authority under the Long-Term Care Homes Act, 2007.
113 Inspectors have broad powers. They can enter a long-term care home at any reasonable time without notice; examine premises, demand, view and copy records, question people, make recordings, remove evidence, call in outside experts, and obtain search warrants if necessary.[88]
114 The Ministry’s Inspections Branch is led by a Director, who has many specific responsibilities and powers set out in legislation. The Branch is further divided into seven regional service area offices, each of which has one Service Area Office Manager, two inspection managers, 22 to 25 inspector positions, as well as some administrative staff.[89] Four senior managers share oversight of the seven service area offices.
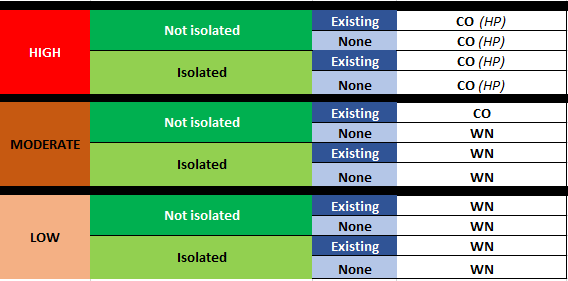
115 The Branch conducts inspections into complaints, critical incidents and open Ministry compliance orders. It can also conduct proactive inspections. Complaints and critical incidents are assessed and given a risk level from 1 to 4, with 4 representing the highest level of risk. Generally, the Branch inspects files with a triage risk level of 3, 3+, or 4. When the pandemic began in March 2020, the Branch was carrying out four types of inspections:
- Complaint inspections: These occur in response to specific complaints about homes filed by residents, their family, or others.
- Critical incident inspections: A “critical incident” is a specific type of event that a home is required by law to report to the Ministry. It includes significant outbreaks of disease.
- Follow-up inspections: These check whether the home has remedied issues that the Ministry previously ordered the home to fix.
- Service Area Office-initiated inspections: These give the Ministry authority to inspect any home on the Ministry’s own initiative.
116 Each home must be inspected at least once per year and inspections are typically unannounced.[90] In the past, the Branch also conducted resident quality inspections or RQIs. These were more comprehensive inspections that examined a standard list of items in the home. However, this type of inspection was resource-intensive and led to backlogs prior to the pandemic. The Branch switched to a risk-based inspection approach and completed its last pre-pandemic RQI in July 2019.
117 The Ministry records inspection findings and related enforcement actions in reports, which are shared with long-term care homes and posted with anonymized resident information on the Ministry’s “Reports on Long-Term Care Homes” website.[91] When the pandemic began, enforcement actions ranged from a written notification, which resulted in no Ministry follow-up, to licence revocation that would force the home to close.[92]
118 Inspectors must be members of a specified regulated health profession, with registered nurses and dieticians the most common. Near the end of the first wave in June 2020, the Branch had 152 inspector positions filled, out of a total of 171 available positions. Ministry officials explained to us that maintaining a lower staffing level was a deliberate decision, resulting from internal financial pressure. The Independent Long-term Care COVID-19 Commission also reported that prior to the pandemic and during the first wave, the Inspections Branch had insufficient funding to staff all of the available inspector positions.[93]
119 In addition to inspectors, at the start of the pandemic, the Branch had three long-term care consultant/environmental inspectors to help advise and support inspectors on various matters, including infection prevention and control and emergency plans and incidents. Historically, these specialists were typically brought in at the request of an inspector after receiving approval from a Branch manager. The environmental inspector’s role was mostly to support, advise, and train other inspectors.
On-site inspections
120 Prior to the pandemic, the vast majority of inspections occurred on-site at long-term care homes with inspectors relying on reviewing records, observation, and interviews to make findings. Off-site inspections, which rely solely on document reviews and virtual interviews, were very rare. Typically, inspections would consider a home’s compliance history for the past 36 months. Using relevant “inspection protocols,” inspectors assessed whether the home was complying with specific legislative provisions. Any findings of non-compliance required evidence from at least two of three sources (interviews, observations and reviewing records). If non-compliance regarding a resident issue was found, the inspector had to expand the review to include three more residents.
121 At the end of an inspection, inspectors would debrief with the home and contact complainants within two business days of completion. They then prepared the inspection report and sent it to the home, usually within 20 business days. Within two business days of sharing the inspection report with the home, inspectors were expected to follow up again with any affected complainant.
Identifying “high-risk” homes
122 Prior to March 2020, the Inspections Branch used a number of methods to identify long-term care homes that might be at higher risk of not complying with the law. This helped focus the Branch’s resources and guide its inspection efforts.
123 One of the main tools used was a scorecard called the Long-Term Care Home Performance Report, which helped gauge the performance of long-term care homes over a period of time, using a specific set of resident indicators. This report identified how many times certain events had occurred, such as findings of non-compliance, high-risk compliance orders, and re-issued compliance orders. It did not identify the underlying issue (e.g., infection prevention and control) that led to each event. The Branch typically shared this report with the long-term care sector every three months, but it is not clear what further action, if any, flowed from this communication.
124 The Branch also relied on a document referred to as the “Director’s dashboard” to identify high-risk homes. This was a list of homes and the status of compliance activities where the Inspections Branch Director was directly involved.
125 Inspectors also told us about other ways that the Branch became aware of homes at higher risk of non-compliance, including discussions at team meetings, trends analyses conducted when reviewing new complaints and critical incidents, and general knowledge of how certain homes performed over time.
Stop inspections, effective immediately
126 As Ontario became increasingly concerned about the spread of COVID-19, on March 13, 2020, the practices of the Ministry’s Inspections Branch shifted dramatically. On that Friday, Ontario’s Secretary of Cabinet instructed members of the Ontario Public Service to work from home wherever feasible. The Ministry of Long-Term Care asked the Inspections Branch to adhere to the Secretary’s direction, and service area office managers passed on the news to inspectors. Although the wording differed, the message was clear: All inspections must immediately stop.
127 On Saturday, March 14, the Inspections Branch Director[94] wrote to all inspectors to confirm that employees would be working from home for three weeks. The Director asked for the inspectors’ patience while the Branch figured out a plan.
128 The senior Inspections Branch officials scrambled to come up with a path forward. The plan they ultimately proposed was contained in a slide deck that set out the following information about inspections:
Proactive Inspections – will be suspended during COVID-19
Reactive Inspections:
- Follow-up Inspections – Low-risk [compliance] order follow-up inspections will be postponed. Inspectors will follow up on high-risk orders (e.g., director orders) using off-site inspection processes wherever possible.
- Complaint Inspections – Inspectors will follow up with all complainants and determine level of risk to residents. There has been an increased volume of complaints related to visitor restrictions. Inspectors have been provided with key messages to assist them on these calls. **Highly recommending the importance to maintain contact with the public regarding complaints.
- Critical Incident Inspections – Inspectors will monitor Critical Incident Intakes and triage levels will be assigned. High-risk intakes will be inspected using most appropriate inspection process. Wherever possible off-site inspections will be used.
- High-risk inspections would encompass situations where there is immediate risk to residents.
The slide deck clarified that high-risk cases “may need in-person [inspection]; off-site inspection may be used.”
129 This information was forwarded to the Deputy Minister’s office for approval on March 17, and on March 21, the Deputy Minister learned that Cabinet Office had “no concerns” with the approach and the Inspections Branch had the “green light to move ahead.”
130 Later that same day, the Premier’s Office asked how many inspections the Branch expected to continue doing. The Branch Director replied that they would continue to carry out inspections of high-risk situations, representing approximately 15% of the Branch’s usual inspection volume. The Director’s response did not specify if those inspections would occur on-site or off-site. During his interview with our Office, the Deputy Minister of Long-term Care said that based on the Branch’s plan, he understood that inspectors would be on-site to inspect the high-risk scenarios.
131 However, the Ministry took a different approach. While waiting for Cabinet’s approval of the plan, the Inspections Branch decided inspectors would only conduct off-site inspections, even for high-risk issues, except in the most “extenuating” circumstances. This was reflected in a separate document (the “Ministry of Long-Term Care Inspection Branch Strategy”) drafted by Branch management. The March 16 version of the strategy said:
The inspection process will be conducted off-site and will be risked [sic] focused.
Note: In extenuating circumstances and only with management approval, an inspector may inspect in a home where there is a significant high-risk situation impacting one or more residents in a home. Proper emergency protocols will be applied.
132 On March 18, the Inspections Branch Director told inspectors that low-risk inspection files would be placed “on hold,” and only high-risk inspections (level 3+ and 4 files) would proceed in a “focused” manner.
133 At approximately the same time (March 18-19), the Inspections Branch put the “COVID-19 Emergency Inspection Policy” in place. It said the Branch would use a standardized approach for conducting “emergency off-site inspections … during situational circumstances, e.g., outbreak or pandemic,” and would be used whenever an inspector was unable to go to a long-term care home to conduct an inspection. The policy confirmed that only high-risk inspections would proceed (levels 3+ and 4), and that they would generally be done off-site, except for extenuating circumstances with management approval.
134 The Director emailed the Assistant Deputy Minister on March 19 that she had “already given the green light to start with [the Branch’s] emergency processes,” a few days before the Premier’s Office and Cabinet Office officially approved the plan on March 21. These policies made it clear that the Branch’s default approach to high-risk situations – even those involving “immediate risk to residents” – would be off-site inspections.
135 In addition to halting new inspections, by March 25, the Branch had also decided to stop doing all follow-up inspections, even if the underlying issue was high-risk. This decision meant inspectors would not check to confirm that the homes had remedied issues from any open Ministry compliance orders.
136 On March 16, the Inspections Branch also stopped issuing completed reports from pre-pandemic inspections. On March 18, it received approval to purchase software that inspectors could use to prepare inspection reports and issue them to long-term care homes electronically – a new process for the Ministry. We were told the Branch created tools to help inspectors use the new software, but installing it on the inspectors’ computers proved difficult. Branch managers initially said they hoped to have this completed by mid-April 2020, but it ended up taking much longer. More than 100 inspection reports sat at the Branch for more than two months, waiting to be issued to the homes. It wasn’t until May 21, 2020 that inspectors regularly resumed issuing reports.
When you fail to plan…
137 If the Inspections Branch had planned ahead for how to continue operating during a pandemic, it might have avoided a situation where all inspections and inspection reports ground to a halt. However, there had been almost no advance planning. The best guidance available was the government’s plan for an influenza pandemic, which was last updated in 2013 and contained nothing about how the Ministry of Long-Term Care would function during a public health emergency.
138 Senior officials we spoke with acknowledged that there was no guidance available to the Ministry about how to respond to a crisis of this nature. One commented that the Ministry was “figuring it out as we went along.” The Inspections Branch Director said the Branch had not prepared for a scenario in which inspectors would be called upon to work during a pandemic. Even between January and March 2020, as information emerged about the developing global COVID-19 threat, the Ministry took no specific steps to prepare for continuation of inspection-related activities.
139 A handful of Branch officials pointed to the Ministry of Long-Term Care’s overall “continuity of operations plan” (“COOP”), which set out basic information on how the Ministry would operate in case of disruption. The Ministry updated its COOP on March 9, 2020 – two days before the World Health Organization declared COVID-19 to be a pandemic. The COOP listed the contact information for key staff and instructions for specific emergency situations for all Ministry areas. One of those situations was “Scenario 3 – pandemic.” It provided the following information for each Inspections Branch office:
- If a pandemic/potential health risk arises, staff will be asked to bring home their laptops, files, etc. home daily in the event they need to work from home – this can be done through VPN or Office365.
- Staff to monitor appropriate pandemic websites and watch their email for updates.
- Staff to take necessary steps to reduce exposure to and transmission of illnesses (e.g., wash hands, cough, sneeze in sleeve, avoid touching eyes, nose, mouth, etc.)
140 There were no further details about how the Branch would conduct inspections during a pandemic or any other emergency.
141 Some of the Branch leaders, managers and inspectors we spoke with questioned why the Branch wasn’t ready for a pandemic. One manager said a lot of pandemic planning work was done in the long-term care sector after the SARS outbreak in 2003, but that “when SARS went away, so did everything else.” Another manager agreed that a plan would have been helpful, and that without one, they were “totally unprepared” and “floundered around not knowing what to do.”
Seven lost weeks
142 Without a clear path forward, the Inspections Branch struggled to figure out how staff would operate after the pandemic was declared. The last-minute plan that was approved by Cabinet indicated that the Branch would continue on-site inspections of high-risk complaints and critical incidents. The direction to inspectors was different. It said high risk inspections would occur mainly off-site, and on-site “with management approval only and in extenuating circumstances.” In reality, as the number of COVID outbreaks increased and 720 related deaths occurred in the long-term care sector during the initial weeks of the first wave, no on-site inspections occurred for seven weeks. One Ministry staff person told us:
We weren’t even going out [to do inspections]. No, this was a really terrible time… this was really terrible. Because we’re getting these calls and we couldn’t – we weren’t, we had nobody to go out to them. We had no direction. It was very bad.
143 Many senior officials, including those in the Minister of Long-Term Care’s office, the Deputy Minister, and the Incident Commander of the Incident Management System Table for Long-Term Care, did not initially know that the Branch had stopped on-site inspections. It was even challenging for my Office to reach this conclusion with the benefit of hindsight. Our investigators closely analyzed many different sources of data and conflicting witness testimony in order to make this determination. Many documents that we were given failed to distinguish between on-site and off-site inspections, or grouped data over long periods to obscure the seven-week inspection hiatus.
144 However, the detailed information provided by each of the Branch’s seven service area offices clearly demonstrates that on-site inspections stopped immediately after March 13, 2020. That same data showed when each office restarted on-site inspections (and “blended” inspections, which include both on- and off-site work):
- Toronto began its first on-site inspection on May 8, 2020.
- Ottawa started on-site activity as part of blended inspections on May 8, 2020, and its first fully on-site inspection on June 22, 2020.
- Central East started its first on-site inspection on May 11, 2020.
- Central West started blended inspections on May 14, 2020, and its first fully on-site inspection on May 20, 2020.
- London began on-site inspections on May 19, 2020.
- Sudbury began on-site and blended inspections on May 20, 2020.
- Hamilton started off-site work for blended inspections on May 19, 2020, but did not go on-site until June 15, 2020.
145 Based on the evidence we reviewed, the earliest on-site inspections restarted on May 8, 2020, seven weeks after they stopped. However, the pause was much longer in some areas. In Hamilton, no inspectors were in the field for three entire months.
146 Outside of the Inspections Branch, few seem to have been aware that inspections had ceased. There was no public announcement, and long-term care homes were not informed. Even many senior government officials were unaware that on-site investigations were not occurring. For instance, as late as May 4, 2020, the Incident Commander for the Incident Management System Table for Long-Term Care asked the Deputy Minister for the number of on-site visits the inspectors had done over the past two, four and six weeks, believing that on-site inspections had been conducted over that time.
147 This confusion and misinformation lasted for many months. For example, in mid-June 2020, senior government officials circulated a briefing note saying the Ministry of Long-Term Care “did not stop on-site inspections during COVID-19.” The Branch suggested changes to this wording. Even months later, some senior Ministry and Branch officials still did not know that on-site inspections had paused. For example, an Assistant Deputy Minister and several senior Branch managers told our investigators that on-site inspections continued throughout the first COVID-19 wave.
148 The Long-Term Care Homes Act required that the Ministry conduct on-site inspections of long-term care homes in certain circumstances, including where there were allegations of:
- Improper or incompetent treatment or care of a resident that resulted in harm or a risk of harm to the resident.
- Abuse of a resident by anyone or neglect of a resident by the licensee or staff that resulted in harm or a risk of harm to the resident.
- Unlawful conduct that resulted in harm or a risk of harm to a resident.[95]
149 Where one of those issues “may” have occurred and the issue “resulted in serious harm or a significant risk of serious harm to a resident,” the Act provided that a Ministry inspector “shall immediately visit the long-term care home concerned.”[96] Similar provisions apply in the new Fixing Long-Term Care Act, 2021.[97]
150 The Ministry was not in a position to carry out critical, legislatively mandated inspections for some seven weeks at the start of the pandemic. This is clearly unacceptable and a significant system failure. In order to properly fulfil its function of protecting the welfare of long-term care residents, it is vital that the Ministry ensure it always has inspectors ready to conduct on-site inspections, including immediately, if the circumstances call for it.
Recommendation 1
The Ministry of Long-Term Care should ensure that the Inspections Branch always has inspectors immediately available to inspect on-site at long-term care homes.
No consequences
151 The failure to conduct inspections also affected the Ministry’s ability to take enforcement action against long-term care homes. The Branch stopped all enforcement activity once inspectors were ordered to work from home and inspections ceased. The Branch Director confirmed this approach in a message to inspectors on March 27, 2020, stating:
I will underscore for everyone that our work and the role we will play moving forward is not going to be one of compliance and enforcement for the time being.
152 There were two reasons the Branch couldn’t take any enforcement action during this period. First, inspections had ceased, which meant that no new non-compliance situations would be identified to allow the Ministry to take enforcement action. Second, inspectors had been instructed not to issue inspection reports to long-term care homes, and these reports are the means through which the Branch communicates its enforcement actions to homes.
153 The Inspections Branch didn’t resume regularly issuing inspection reports until May 21, 2020. By this point, enforcement action had essentially been abandoned for more than two months.
Off-site inspections
154 During the seven weeks that on-site inspections did not take place, there were also very few off-site inspections. At the start of the pandemic, the Inspections Branch had no specific policy for conducting off-site inspections. By March 19, 2020, the Ministry had quickly drafted a document that provided guidance on how to conduct a focused off-site inspection based on interviews and record reviews. However, inspectors didn’t have an established process or experience to draw from. On March 25, the document was amended and rebranded as the “Emergency Off-Site Inspection Policy.”
155 No off-site inspections took place in March. By April 3, senior Branch managers were considering off-site inspections for some specific high-risk complaints, but no off-site inspections resulted from their discussions at that time.
156 Two weeks later, on April 17, one senior Branch manager wrote to colleagues saying the Branch was starting to do off-site inspections for cases that “we can possible [sic] resolve with phone calls.” However, based on the data we have from the service area offices, the Branch did not start any formal off-site inspections that week. A Ministry email stated that inspectors had focused on other activities.
157 The following week, the Hamilton service area office started two off-site inspections – one on April 21 and the other on April 24. No other inspections were conducted in April.
158 A week later, on May 1, the Branch sent a slide deck to senior Ministry officials recommending inspections for several specific high-risk matters. The deck did not specify whether those inspections would happen on- or off-site. About a week later, a senior Branch manager sent inspectors a new guidance document regarding inspections for the highest-risk situations, called “High Risk Intakes Process during COVID-19 for intakes that are 3+ and 4.” It said inspectors were to proceed with inspections for any level 3+ and 4 files, whether or not the home was in COVID outbreak, and that level 3 files would remain “on hold until further notice.” It also noted that off-site inspection processes were to be prioritized, with on-site inspections only allowed with management approval. Off-site inspections began at all service area offices shortly after. There were no level 4 complaints during the first wave, but one level 3+ file included a complaint that a resident had passed away as a result of being fed by staff while the resident was lying down, and a level 3 file alleged that a resident had died from an unknown cause of death, with potential non-compliance around infection prevention and control.
159 Off-site inspections presented many new challenges at an already challenging time. Inspectors told us it is often impractical to speak by telephone with long-term care residents, some of whom have hearing issues or who do not have a private place to take calls. One described an inspection that predated the pandemic but had to be restarted as an off-site inspection in May 2020. The inspector said the affected resident had substantial verbal communication challenges. The inspector said they appealed to management for permission to do the inspection on-site but was unsuccessful. Ultimately, the resident left the home before the inspector was allowed back in. They told us that when they did finally visit the home, they were distressed with the conditions they witnessed.
160 We also heard from inspectors that it was difficult to access long-term care homes’ records off-site. One region told us that its inspectors had remote access to long-term care homes’ records early in the pandemic, but at a later point, inspectors had to ask the home to print out the relevant records and pick them up in person. Some inspectors also felt that their requests for records were not prioritized, affecting the timeliness of the information they received.
161 While off-site inspections were perhaps better than none, many we spoke with had serious concerns about their effectiveness. One very senior government official told us that when he heard that inspectors were not going into homes, “my head popped off. Like, how do you do a virtual investigation of a long-term care facility?” He expressed concern that the worst homes were not being honest about what was going on. He also felt that an off-site or “virtual” inspection “does not signal to the home the seriousness with which we take this, this responsibility. And it doesn’t signal to the staff that we’re going to uncover problems and fix them.”
162 Many stakeholders we spoke with agreed that inspectors needed to be in the homes to see what was happening firsthand. The province’s Incident Management System Table came to a similar conclusion in July 2020 during a “lessons learned” discussion, noting:
It is difficult to assess homes virtually - virtual assessments could be a supplement to onsite visits but alone they are not adequate. When a home or a resident is in crisis, their environment cannot be assessed fully without an onsite visit.
163 As of February 2022, the Inspectors’ Handbook still had an “Off-Site Inspection Policy.” Its preamble says:
Complaint, Critical Incident System (CIS), and Follow-up (FUI) inspections are by default, conducted on-site of the long-term care home (LTCH). In situations where an emergency, e.g., flood, fire, or a pandemic, is declared, the inspection can be conducted off-site, if the inspector is able to gather all information required to determine compliance through interviews and record reviews.
164 The policy outlines some factors that Branch management should consider in deciding if an off-site inspection is appropriate. It notes that any “level 4” files or contentious issues must be inspected on-site, and a manager must approve any off-site inspection. The Ministry told us that despite the wording of the policy, off-site inspections can be used in non-emergency situations, taking into account such factors as the nature of the issue being inspected, level of risk, and sources of information. We were told that an inspector can determine if on-site observations are necessary, and change the inspection accordingly.
165 Although there may be some issues that are appropriate for off-site inspection, the Ministry’s own records reflect that they are normally rare. The Ministry of Long-Term Care should implement a policy that clearly sets out what types of issues can be inspected using an off-site process, or a blended off-site and on-site approach. The policy should also identify circumstances where an on-site inspection is always required. To operationalize this policy, the Ministry must work with long-term care homes to ensure that the Inspections Branch can remotely access long-term care homes’ records without delay. There should also be specific procedures for remotely interviewing long-term care staff or residents, which take such things as video communication and the need for privacy into consideration. Off-site inspections should be the exception rather than the norm, but these steps will help ensure that inspectors and long-term care homes are prepared if they are needed.
Recommendation 2
The Ministry of Long-Term Care should establish a policy clearly setting out what types of issues can be inspected using an off-site process, or a blended off-site and on-site approach. The policy should also identify circumstances were an on-site inspection is always required.
Recommendation 3
The Ministry of Long-Term Care should work with long-term care homes to ensure that the Inspections Branch can remotely access long-term care homes’ records electronically without delay.
Recommendation 4
The Ministry of Long-Term Care should work with long-term care homes to establish a procedure for remotely interviewing long-term care home staff or residents that considers the importance of privacy and video communication.
Difficulties in restarting inspections
166 We heard several explanations for why it was necessary to pause inspections, and why it took so long for them to resume. The Branch Director told us that inspectors were not prepared for a pandemic, so they did not have infection prevention and control (IPAC) training that would allow them to safely put on and take off the medical equipment necessary to keep themselves and others safe. The Inspections Branch Director told us that prior to the pandemic, the training program for new inspectors did not cover IPAC or personal protective equipment (PPE) because there “wasn’t a need” for this type of training.
167 Initially, there was also no personal protective equipment available to inspectors even if they did know how to use it. The Inspections Branch also had no strategy for testing inspectors for COVID-19, or scheduling them to ensure they weren’t inadvertently spreading the virus between long-term care homes.
168 The inspectors' union strongly advocated to have these issues considered and resolved before on-site inspections resumed. The union president stated in an April 22, 2020 email that “risking the health of residents and inspectors [by restarting inspections] has zero value right now.” The Deputy Minister told us the government spent “at least two weeks” trying to satisfy the union’s concerns and reach mutual consensus. We were told this was not possible, as the union did not support on-site inspections under any circumstance the Ministry could offer. Senior Ministry officials told us inspections would have restarted sooner if supported by the union. Our investigation found no evidence that the union or individual inspectors ever participated in a work refusal, although it is clear that various concerns, including those expressed by the union, impacted the resumption of on-site inspections.
169 Ultimately, the Ministry co-ordinated with Public Health Ontario to train inspectors on how to properly use PPE, and on general infection prevention and control measures. This training occurred on April 21, 2020. A senior manager told us the partnership was necessary because the Ministry did not have its own IPAC and PPE experts. On April 30, the Branch created a form that each inspector had to sign indicating they had completed the training. This training was required before inspectors were allowed to return to on-site inspections, and it is now mandatory for all inspectors to complete it every six months.
170 In mid-April 2020, the government was experiencing a severe shortage of PPE, and long-term care homes in crisis were struggling to get more than a few days’ supply. To ensure the PPE went where it was needed most, the province’s Control Table had a framework to prioritize what was available, and that framework made no mention of long-term care inspectors. On April 16, the Branch asked the Ministry to allocate PPE to inspectors. On April 21, it was told that inspectors could get masks and gloves, but the available gowns were “aged,” the shields/goggles were “expired”, and there was “no stock” of wipes or sanitizer. However, by April 29, the Branch had sourced the required PPE despite the provincewide shortage. These supplies were couriered to individual inspectors with a delivery date of April 30, and at approximately the same time, the Branch sent inspectors a document outlining protocols for using the PPE. Ministry officials, including the Deputy Minister of Long-term Care, acknowledged to us that the delay in getting PPE to the inspectors affected the resumption of inspections.
Testing and isolation
171 The Branch also grappled with testing inspectors for COVID-19 during the first wave. Testing capacity was very limited at the time, and results were slow to arrive. The Branch told inspectors they could get tested at assessment centres, but they were not required to do so, and their results were not prioritized by the provincial system. By early July 2020, the Branch issued guidance to inspectors through a “’Q&A” document, stating that it was “possible” for inspectors to get tested, and suggesting any inspector who needed a flexible work arrangement in order to get a test should speak to their manager. The same document confirmed that inspectors could move between long-term care homes as long as they wore proper PPE and adhered to all IPAC practices.
172 Meanwhile, some homes tried to impose their own testing requirements on inspectors before allowing them to enter. This approach was not supported by Inspections Branch management, who noted that the long-term care legislation required homes to allow inspectors access without delay.
173 Eventually, in December 2020 – deep into the second wave – the Ministry began requiring inspectors to get tested regularly. As of December 16, 2020, inspectors entering homes in regions with heightened restrictions were required to get a COVID test every week; those entering homes in other regions had to be tested every two weeks.
174 To ensure that it is prepared for any future pandemic or disease outbreak, the Branch should work with relevant government organizations to develop and codify its approach to testing long-term care home inspectors. This policy should be shared with the long-term care sector, the union representing inspectors and other stakeholders.
Recommendation 5
The Ministry of Long-Term Care should work with relevant government organizations to develop a policy on requirements for infectious disease testing for inspectors.
Recommendation 6
The Ministry of Long-Term Care should share the policy referred to in Recommendation 5 with the long-term care sector, the union representing inspectors, and other stakeholders.
175 As it was figuring out its practice relating to testing inspectors, the Ministry did not put any restrictions on the homes that they could visit. In fact, the Ministry’s policy said inspectors could move immediately between a long-term care home experiencing a COVID outbreak and another that was not in outbreak. This is in contrast to long-term care home staff, who were eventually restricted by government directive to working at only one home.
176 The Ministry’s approach, combined with its decision to not require testing for inspectors, increased the risk that inspectors could spread COVID from one home to another. Many inspectors and long-term care homes expressed concern about this, and some homes tried unsuccessfully to require inspectors to submit to testing before allowing them entry. We heard that some service area offices were attuned to the risk of transmission between homes and made inspectors wait 14 days after visiting a home in COVID outbreak before visiting another. However, this was not a universal practice.
177 To reduce the risk that Ministry inspections will spread infectious diseases during acute outbreaks, the Branch should develop a policy setting out how and when inspectors will be permitted to move between homes when they have visited a home experiencing an outbreak of infectious disease.
Recommendation 7
The Ministry of Long-Term Care’s Inspections Branch should develop a policy covering movement between long-term care homes when inspectors have visited homes experiencing outbreaks of infectious disease.
The future of long-term care inspections
178 In the time since the first wave decimated long-term care homes and brought the work of the Inspections Branch to a halt, the Inspections Branch has taken steps to better prepare itself to respond to a future pandemic and other emergencies. Much of this planning is contained in a policy called “Preparing for On-Site Inspections During a Pandemic,” and a similar policy has been developed for other emergencies.
179 For the pandemic-specific policy, the preamble explains that a pandemic could pose a risk to inspectors’ safety, and that Ministry inspections “are considered an essential service and must continue safely during a pandemic.”
180 According to the policy, each August every service area office must go through a checklist to ensure:
- They are aware of any updates to Ontario Public Service/Ministry pandemic plans and that all communication channels in those plans are current.
- New and existing staff are trained on how to inspect during a pandemic (inspectors are required to go through the training every six months).
- Every service area office has a three-month supply of personal protective equipment (staff must check that the PPE is not expired; staff will be fit-tested for N95 masks every two years).
- They have up-to-date contact information for all organizations the Inspections Branch would be in regular contact with during a pandemic.
181 The document also sets out a longer checklist that the Branch must follow when there are signs of a possible pandemic. The additional requirements include:
- Procuring specific PPE the Branch might need for the specific pandemic;
- Providing necessary training focussed on the specific disease;
- Identifying how many back-up inspectors the Branch might need; and
- Using the precautionary principle, if necessary, to reduce risk even when a pandemic has not been officially declared. (In this context, the “precautionary principle” means that inspectors should take enhanced steps to protect themselves and others while the threat of disease is being determined and studied.)
182 There is a similar checklist for the Branch to follow when a pandemic arrives, and a checklist to review after a pandemic for debriefing and lessons learned. However, despite all these details, the policy doesn’t explain how the Branch will decide whether on-site or off-site inspections should be used during a future pandemic, and what safety factors the Branch might consider in making that decision.
183 This policy is a step in the right direction, but it is concerning that the Branch has not established a framework for determining whether inspections during a future pandemic should occur on-site or off-site. Without criteria, Branch management could easily find themselves in a similar situation to mid-March 2020 – unsure what to do as the crisis unfolds around them. The Ministry of Long-Term Care should amend its policy so it is clear about when inspectors will work on- and off-site during a pandemic and similar crisis situations, and what criteria will affect that decision. The policy should also establish who will be responsible for making these decisions and how they will be communicated to long-term care homes and the public. This preparation will help ensure the Branch is ready to act when the next pandemic begins.
Recommendation 8
The Ministry of Long-Term Care should amend its Preparing for On-Site Inspections During a Pandemic policy so it clearly defines when inspectors will work on- and off-site during pandemics and similar crisis situations, and what criteria will factor into that decision.
Recommendation 9
The Ministry of Long-Term Care should also amend this policy to establish who will be responsible for making criteria-based decisions about on-site versus off-site inspections during a pandemic and how these decisions will be communicated to long-term care homes and the public.
184 Similarly, the Inspections Branch’s new requirement that every service area office have a three-month supply of personal protective equipment is an important step to ensure that inspectors can continue their work when the next pandemic arrives. However, beyond setting this high-level goal, the Ministry must ensure that it has the infrastructure in place to make PPE preparedness an ongoing reality.
185 To ensure it is prepared for a future pandemic, the Ministry should develop and implement a specific policy regarding the procurement, storage, and use of personal protective equipment. The Ministry should ensure that its approach will provide inspectors with adequate supplies of PPE to continue operations, even during periods of acute shortage where it may not be possible to easily replenish existing stockpiles. The Ministry should also proactively engage with other provincial organizations responsible for managing strategic PPE supplies to ensure that the needs of inspectors are appropriately prioritized in the case of a future pandemic.
Recommendation 10
The Ministry of Long-Term Care should develop and implement a specific policy regarding the procurement, storage, and use of personal protective equipment (PPE). The Ministry should ensure that its approach will provide inspectors with adequate supplies of PPE to continue the Ministry’s operations even during periods of acute shortage.
Recommendation 11
The Ministry of Long-Term Care should also proactively engage with other provincial organizations responsible for managing strategic PPE supplies to ensure that the needs of Ministry Long-Term Care inspectors will be appropriately prioritized in the case of a future pandemic.
New Priorities for Inspectors
186 When inspections were paused during the first wave, Ministry officials found another way to keep inspectors occupied. After some discussion, on March 28, 2020, the province issued a news release summarizing how the inspectors’ role would be changing. It explained:
The Ministry of Long-Term Care is also implementing a new approach to redeploying its highly qualified inspectors. These nurses, dieticians, and physiotherapists will be supporting long-term care homes on the ground through staff supply, care co-ordination, serving as point-people with Public Health, helping homes to prevent and contain infections, and many other tasks necessary to the safety and security of residents.[98]
187 This announcement proved to be overly optimistic, and three weeks later, no inspectors had been sent to provide homes with “on the ground” support. A number of practical issues, such as the need for training and access to PPE, remained unresolved. Ultimately, no inspectors were redeployed to directly provide assistance to homes.
188 However, inspectors did end up supporting the homes in other ways. A new process called “support and monitoring calls” meant that inspectors spoke regularly with most of the homes to collect information about their situation.
189 On March 17, 2020, the Inspections Branch sent a slide deck to the Deputy Minister’s office that explained what it was planning to do:
- Support and Monitoring to Homes – Inspectors will play a critical role in collecting information to feed through to the appropriate tables to trigger support for homes where needed. The key areas of monitoring include:
- Residents or staff with confirmed or potential COVID-19
- Staffing shortages
- Work refusals
- PPE supply shortages.
The slide deck confirmed that inspectors would be “proactively reaching out to long-term care homes and regularly monitoring to ensure the health and safety of residents during COVID-19.” The Inspections Branch Director told us this new role was only supposed to exist for “a very short period of time,” and that the Inspections Branch took on the responsibility because no one else had the “appetite” for it.
190 On March 18, the Inspections Branch Director wrote to all Branch staff, indicating that the Branch was working on assigning pairs of inspectors to support and monitor every long-term care home. Staff were asked to communicate regularly with the homes they were assigned to and check in on how they were coping with COVID-19. Most inspectors were assigned approximately four homes, although some recalled having as many as 10. The Ministry did not do any outreach to homes to let them know that inspectors would start making these calls.
191 The Branch Director suggested twice-weekly calls, and instructed inspectors to provide homes with their contact information. The Director also asked inspectors to limit the time they spent speaking with the homes, and to specifically reassure the homes that “this is not a compliance exercise.”
192 This new approach was approved by Cabinet Office on March 21. The Inspections Branch created a policy document to outline this new role, called the “COVID-19 Support, Monitoring and Triaging Policy.” The March 25, 2020 version noted inspectors were to follow a “standardized approach” in making their calls to the homes, although it provided few additional details beyond what had already been communicated. Inspectors were to call homes “to offer support and monitor how they are coping,” and to monitor respiratory and COVID outbreaks. Inspectors were instructed to ask specific questions and report what they learned in a centralized “tracker” document, which requested such details as:
- Whether the home was in COVID outbreak;
- Number of resident and staff COVID cases;
- Any staff shortages;
- Any work refusals;
- Any shortage of personal protective equipment; and
- Any issues around visiting restrictions.
193 The policy included a list of specific questions to guide inspectors’ conversations, as well as a script for the first call. It also indicated that inspectors should ask homes if they wished to keep receiving these calls, and if so, to establish how often and the preferred method of contact.
194 We were told inspectors made about 1,000 support and monitoring calls to long-term care homes each week during the early part of the first wave. Many, but not all, homes accepted the “support and monitoring” provided by the Inspections Branch staff, although some expressed concern about giving information to inspectors that could later be used against them in an inspection.
195 A few large long-term care chains, including Extendicare, Sienna Senior Living, and Jarlette, initially did not engage with the Ministry’s initiative. They had numerous homes – likely more than 100 in total. Later, some did provide one “corporate response” to the Ministry each day. It is unsurprising that some homes were hesitant to participate in these calls, given the challenging circumstances they faced, and the lack of clarity about the purpose of the calls. We were told that the line between compliance-related work and “support and monitoring” was not always clear, and the sector received mixed messages. For example, we heard that in many cases, inspectors made inquiries about specific complaints during their “support and monitoring” calls. Some homes also expressed concerns that the calls cut into time needed to care for residents, and that the support and monitoring process duplicated information that was already being collected in other ways, such as reporting to public health units. Some of the inspectors who made the calls told us they too felt the calls collected information that was already being reported in other ways. The twice-weekly calls decreased over time, and eventually the frequency of calls was based on the risk that COVID posed to each home. Late in the first wave, this approach was codified in Ministry policy, which linked the frequency of calls to various levels of COVID risk.
Data overload
196 The data collected from the Ministry’s support and monitoring calls was entered by inspectors into a tracker document and converted into a report. We were told that the report was based solely on self-reported data from the homes, and there was no attempt to verify the accuracy of the information.
197 Nevertheless, within a day or two of its creation, the Branch’s report was being shared quite broadly within the government. According to senior Ministry officials, the report was instrumental in the government’s assessment of the risk that COVID posed to each home, especially in the initial days of the pandemic.
198 In addition to entering data in the tracking document, when the Branch learned about a COVID outbreak, Branch managers sent a “heads-up” email to senior government officials, with details of the home’s situation and reported needs. As the situation at a particular home changed, Branch staff would circulate an updated email. As the number of COVID outbreaks surged in April 2020, so did the number of these emails. The Assistant Deputy Minister of Long-term Care Operations told us that, like the tracker, the information in the emails contributed directly to the risk level the government assigned to each home. The Assistant Deputy Minister said the Incident Management System Table for Long-Term Care also discussed the content of these emails.
Escalating concerns
199 As well as providing data to decision-makers, the Inspections Branch told us the support and monitoring calls sometimes prompted officials to escalate efforts to get help for specific homes.
200 For example, the Branch Director described contacting the Ministry of Health’s Emergency Operations Centre to try to get personal protective equipment for homes in dire need. The Director also recalled contacting various organizations about staffing shortages at specific homes.
201 One large long-term care operator told us it was helpful to have this type of support, and that Ministry of Long-Term Care inspectors were sometimes effective in helping homes get PPE during critical periods in the first wave. However, we also heard that some homes found the Ministry unhelpful.
Supporting Orchard Villa
202 For Orchard Villa, a 233-bed long-term care home in Pickering, support and monitoring calls failed to identify that it was in desperate need of assistance. Orchard Villa experienced its first COVID case in early April 2020. The local public health unit declared an outbreak at the home on April 13, and told the Ministry the same day.
203 On April 14, the “heads-up email” from the Inspections Branch outlined what inspectors had learned about Orchard Villa’s situation. It listed, in part:
- 50 residents confirmed positive for COVID-19, 17 residents pending results.
- 7 staff confirmed positive
- The home has initiated outbreak management protocols
- No PPE or staffing shortages reported at this time
- Home is managed by Extendicare Assist and supporting the home.
204 The same day, the public health unit organized a call to update various partners, including the ministries of Health and Long-Term Care, on the situation at Orchard Villa. According to a Ministry of Health email about that call, public health said “at minimum, 40 staff are home in self-isolation” and other staff members had “refused to work due to anxiety and fear.”
205 Despite this concerning information, internal email correspondence at the Ministry of Long-Term Care in the following days indicated that they believed the situation was under control. There was substantial inconsistency in the information reported during the daily support and monitoring calls. The home provided conflicting reports – saying there were no PPE or staffing shortages on one day, and that they were short of both PPE and staff the next.
206 Unbeknownst to the Inspections Branch, on April 17 the CEO of the company that owns Orchard Villa wrote an urgent letter to the Local Health Integration Network’s[99] Regional Lead, requesting a rapid deployment team to Orchard Villa. The CEO said the home urgently needed five registered nurses, 10 registered practical nurses, 20 personal support workers, 15 health care aides, and 10 dietary aides – 60 staff in all.
207 The CEO copied the Minister of Long-Term Care, the Ministry’s Director of stakeholder relations, several officials at local hospitals, and others. But, based on the list of “cc” entries at the end of the letter, the CEO did not copy anyone in the Inspections Branch. As a result, the Branch seemingly remained oblivious to how dire the staffing situation had become, and in a spreadsheet prepared the following day, it specifically noted that Orchard Villa did not have “critical shortages” of PPE or staff.
208 It took several days – until April 20 – and several forms of communication for the scale and impact of the staffing crisis at Orchard Villa to become evident to the Inspections Branch. First, the letter from the CEO seeking urgent help was forwarded to the Branch by the Minister’s office. Then the Inspections Branch Director received the results of an infection protection and control assessment done by a local hospital on April 18. It identified serious staffing concerns and suggested that the army, Canadian Red Cross, or hospital staff be brought in for urgent assistance. Finally, a member of Orchard Villa staff told a Ministry inspector directly that there were no staff left to feed and care for residents, and living conditions were like “hell.” This information rapidly made its way to senior Inspections Branch management, who quickly became involved in calls to the home and its operator.
209 By the following day, the gravity of the situation had prompted both local and provincial governments to take drastic action. Durham Region’s Medical Officer of Health issued an order under the Health Protection and Promotion Act, requiring a local hospital to assist the home. This was the first “local order” issued for any long-term care home during the pandemic. In his testimony to the Long-Term Care COVID-19 Commission, Durham Region’s Local Medical Officer of Health said he realized urgent action was needed at Orchard Villa, and that he had notified the Ministry of Long-Term Care about the outbreak a week before issuing his order. He added that the Ministry’s Inspections Branch was “basically missing from action and invisible,” which meant he had to issue his own order.
210 The Ministry of Long-Term Care, the Ministry of Health, and the Canadian Armed Forces (CAF) met to discuss how the CAF could help support long-term care homes. Shortly after that meeting, the government formally requested the CAF’s assistance for Orchard Villa and four other homes. The CAF team arrived at Orchard Villa one week later, on April 28, 2020.
211 The hospital and CAF support helped stabilize the home and improve staffing levels. However, it wasn’t until June 11 that the public health unit declared the home’s outbreak over. In all, the virus took the lives of 70 residents – more than in any other Ontario home during the first wave.
212 On June 13, the Ministry of Long-Term Care signed off on a voluntary management contract for the home, although the outbreak was over. The same hospital that had previously provided support took over management of Orchard Villa for 90 days.
213 The Branch’s support and monitoring process was poorly equipped to sound the alarm about the unfolding crisis at Orchard Villa. Other organizations such as the local health integration network, Ontario Health, and the local public health unit were better placed to identify and warn about what was happening and to help the home obtain the resources it needed. The support and monitoring strategy did not give the Branch any real insight into the rapidly shifting conditions at Orchard Villa, and in the end the Branch was among the last to learn of the desperate situation.
Support and monitoring into the second wave and beyond
214 After inspections resumed in May 2020, the Inspections Branch asked inspectors who were not conducting on-site inspections (due to accommodations for medically-related and other limitations) to continue the support and monitoring function. That approach created a somewhat clearer distinction between the compliance work of the Inspections Branch and its support and monitoring role.
215 As of 2022, support and monitoring calls were continuing for homes in COVID outbreak or for those deemed at high risk of outbreak. However, changes were made to the process after the first wave of the pandemic. Inspectors typically scheduled “outbreak management team” calls that included representatives from the Ministry, Home and Community Care Support Services, the local public health unit, and the home that was in outbreak. We heard that staff from the Inspections Branch sometimes led these meetings, which are intended to streamline communication between the long-term care home and oversight and regulatory bodies.
216 When support and monitoring calls were first implemented, they were an extraordinary response to an emergency situation. The Ministry of Long-Term Care, and the government more generally, needed quick access to accurate information about hundreds of long-term care homes. A solution had to be put in place quickly, even though it was far from perfect. If future situations arise in which the Ministry needs to collect information from homes to monitor and respond to emergency conditions, it should avoid the potential for confusion and conflict by assigning the work to individuals who do not work in a compliance function in the Inspections Branch. It should also co-ordinate with other organizations that are collecting or have access to similar information, such as local public health units, to ensure there is better communication and information sharing and no unnecessary duplication.
Recommendation 12
The Ministry of Long-Term Care should ensure a clear separation of responsibilities so that functions that don’t involve inspections/compliance work are not done by inspectors, to avoid confusion and conflict regarding the inspection function.
Recommendation 13
If the Ministry of Long-Term Care requires data from long-term care homes to monitor and respond to emergency conditions, it should co-ordinate with other organizations that may be collecting or have access to similar information, to ensure there is better communication and information sharing and no unnecessary duplication.
Chaotic Complaint Process
217 At the outset of the pandemic, there was a significant increase in complaints identifying serious issues in long-term care homes – issues requiring inspection. Some of the most critical issues our investigation uncovered related to how the Ministry’s Inspections Branch handled complaints during the pandemic’s first wave. The Ministry’s attempt to pivot away from on-site inspections, along with fundamental changes to its complaint intake process, led to a system breakdown that left it largely unresponsive to multiple, serious issues affecting the safety of long-term care residents.
218 The Ministry was unprepared for a deluge of COVID-related complaints and provided inspectors with limited guidance about how the pandemic should affect the triage and risk assessment process. Concerns about COVID-related infection prevention and control, personal protective equipment and staffing were rarely considered high risk. Moreover, the surge in complaints exposed serious issues in documentation and communication practices at a time when the Branch most needed accurate and complete information.
Complaints before the pandemic
219 Prior to the pandemic, one way for concerned individuals to raise issues with the Ministry was through its complaint line, known then as the “Long-Term Care ACTIONline.” Complainants could also write to the Director of the Inspections Branch. Long-term care homes are also required to have a complaints process, and to forward written complaints directly to the Ministry if they relate to resident care or the operation of the home.
220 The Inspections Branch was responsible for assessing, triaging and inspecting homes based on these complaints. Prior to the pandemic, the Ministry received about 4,000 complaints annually. Much of the Inspections Branch’s activity is triggered by complaints. For example, in 2019, more than a third of all Branch inspections were the result of complaints.
221 The vast majority of complaints the Branch received came through the ACTIONline. Calls to the ACTIONline are answered by ServiceOntario staff, and complaint files are transferred to the Ministry of Long-Term Care. Prior to the pandemic, the Centralized Intake, Assessment and Triage Team within the Inspections Branch was responsible for conducting intake and triage work on all new complaint files. The team typically had 9-10 assessment and triage officers, as well as a team lead.
222 The Inspections Branch had a detailed policy for how its staff should review and respond to a complaint. The key steps have remained the same since the start of the pandemic.
223 First, a triage officer shepherds the complaint through a “complaint assessment and triage” process. Staff create a complaint file in the Ministry’s system that includes all the information received, then the triage officer contacts the complainant to confirm relevant details. At the start of the pandemic, Ministry staff had two business days to do this.
224 After speaking with the complainant, the triage officer must decide if the complaint relates to potential non-compliance with the legislation. Some complaints, e.g., about the cost of parking at a home, do not relate to legal requirements that the Inspections Branch can inspect. If the issue is outside the mandate of the Branch, staff will explain this to the complainant, provide relevant referrals, and close the file.
225 If there is potential non-compliance, the triage officer must assess the overall level of risk related to the potential non-compliance and assign a “triage risk level.”
226 The Branch has a guidance document that sets out the five triage risk levels, and how quickly the inspection or inquiry should begin for each risk level. Branch officials can amend the triage risk level later if the information changes. The levels are:
LEVEL 1 No Harm OR No Risk
A situation that has caused no negative impact on the resident(s) and poses no risk of harm to the resident(s).* An inquiry within 90 business days is considered reasonable.[100]
LEVEL 2 Minimal Harm OR Minimal Risk
A situation that results in minimal discomfort to the resident(s) and/or minimal risk of harm.* An inquiry within 90 business days is considered reasonable.
LEVEL 3 Actual Harm OR Actual Risk
A situation that results in actual harm to the resident(s) which will not resolve without further intervention and/or actual risk of harm OR where there is a pattern of incidents contributing to the harm/risk. This may include a situation involving actual harm/risk where action was taken by the licensee/[long-term care home] staff to minimize the risk or prevent the situation from recurring or escalating. An inspection within 60 business days is considered reasonable*.
LEVEL 3+ Significant Actual Harm OR Significant Actual Risk
A situation that results in an outcome that had a serious negative impact on one or more residents’ health, quality of life and/or safety, or that is creating a serious risk of significant actual harm OR significant actual risk related to one or more residents’ health, quality of life and/or safety. An inspection within 30 business days is required [...]
LEVEL 4 Serious Harm OR Immediate Risk
A situation that places a resident or group of residents in immediate jeopardy (risk) as it has caused (or is likely to cause) serious consequences, injury, harm, impairment, and/or could result in death or did result in death to a resident(s) receiving care in the [long-term care home]. This also includes a situation that the licensee is not taking immediate action to appropriately rectify the issue or has failed to intervene, to prevent the situation from unfolding. This level includes situations that require an immediate visit to the [long-term care home].
Immediate Inspection
An “immediate inspection” […] is required for the following that resulted in serious harm or a significant risk of serious harm to the resident:
- improper or incompetent treatment or care of a resident;
- abuse of a resident by anyone, or neglect of a resident by the licensee or staff;
- unlawful conduct.[101]
[All bold text, italics and underline emphasis is original to the document.]
227 The triage risk level helps the Branch determine what to do next. Generally, for unresolved level 1 and 2 complaints, an inspector makes an inquiry with the home, but does not conduct an inspection. However, before the inspector speaks with the home, a triage officer will search the Ministry’s system to see if the same issue was reported three times for that home in the previous six months (including the new complaint). For anything resident-centred, the issue is considered a “trend” if it has been reported for the same resident three times within six months. If an issue is deemed to be a trend, the triage officer changes the risk level of the file to 3, and assigns it for inspection.
228 Other complaints that are initially assessed as level 3 or higher usually result in an inspection. The higher the level, the faster the inspection should begin. There is no set standard for how quickly the inspector should finish an inquiry or inspection.
As COVID-19 hit, complaints and questions rose
229 In the period leading up to the pandemic, the Branch typically received 250-400 complaints per month, roughly 300 on average. In March 2020, that number surpassed 600 as the government introduced restrictions on long-term care homes and individual homes began experiencing COVID outbreaks.
230 In mid-March 2020, in the face of the rapidly increasing volume of questions, information requests and complaints, the Inspections Branch made several changes to its intake and triage processes. On March 18, it transferred the intake responsibility from its Centralized Intake, Assessment and Triage Team to the inspectors at local service area offices. Inspectors became directly responsible for contacting complainants and deciding on next steps. This change left triage officers with a very limited administrative role for new complaints.
231 The Inspections Branch Director told us she was responsible for this new process, and that she felt it was important to have inspectors make initial contact with complainants once the pandemic began. She noted that all inspectors are health care workers, with the power to get information from the home. She also said the change meant complainants wouldn’t have to speak with multiple people about their concerns (previously, telephone complaints were handled by a ServiceOntario staffer, a triage officer, and an inspector).
232 This new approach further altered the role of inspectors during the chaos of the early pandemic. Instead of their traditional inspection role, they were now also responsible for conducting intake calls with complainants, as well as making support and monitoring calls to long-term care homes. Meanwhile, triage officers were asked to take on a data-entry project during the first wave that was entirely unrelated to the ongoing pandemic. They did not return to their intake role until the end of 2020, when they began to report directly to the service area offices.
233 The accompanying graph shows the number of complaints in 2019 and early 2020, compared to the early months of the first wave:
Number of complaints received by the Inspections Branch, by month, from Jan. 2019 to May 2020.
234 By April 2020, the Ministry was receiving almost four times more complaints than usual as COVID infections rose. The complaint volume numbers began to fall in May 2020, as many first-wave COVID outbreaks were resolved, although complaint levels remained much higher than normal through the rest of the first wave.
235 The impact of rising complaint volumes was felt unevenly throughout the province, in contrast to before the pandemic. The Toronto service area office saw a much higher proportion of complaints than normal during the first wave – at its peak, more than double that of any other office. This put a lot of pressure on the inspectors in Toronto and eventually prompted the Branch to ask inspectors from other areas to help out.
236 Although the increase in complaints was immense, some we spoke with felt these numbers were somewhat misleading, as many of the “complaints” actually involved callers asking questions or seeking information or reassurance. The Branch did not distinguish specific complaints from information-seeking calls. In any event, both types of calls contributed to staff workload, and Branch staff noted that dealing with those seeking information was also time-consuming and challenging.
From ACTION to support
237 At the same time that the role of inspectors and triage officers was changing, the Ministry of Long-Term Care also renamed its complaint line. In the early weeks of the pandemic, the Ministry “repurposed” its complaint ACTIONline as a “Family Support Line.”
238 In a slide deck prepared for senior officials around March 17, 2020, the Inspections Branch explained the change as follows:
Action Line to be repurposed as a family support line – Inspectors will be managing the support being provided to families and working with the homes directly where necessary. We will monitor daily volumes of incoming calls related [to] COVID-19.
239 The “support” was a reference to the “support and monitoring” calls that the Inspections Branch was making to long-term care homes. The Deputy Minister for Long-Term Care told our investigators that the overall intent was to support both the homes and families who were calling the Ministry with questions.
240 The Minister of Long-Term Care tweeted about the name change on April 3, 2020. The graphic attached to the tweet called it the “Family Support and Action Line” – combining the old and new names into one.[102] The Minister said anyone who called would reach an experienced long-term care home inspector “who can answer questions, help you find solutions, or even just have a chat. They are here to help as we face this ever evolving pandemic.” The Inspections Branch Director informed staff of the new name on April 6.
241 While most Inspections Branch officials didn’t offer us views on this new approach, the few who did had concerns. For example, one inspections manager expressed disagreement with the name change because the Branch does not provide “support,” it does inspections. A long-term care home resident echoed this sentiment, telling us: “I’m not looking for support. I’m looking for action.”
Key messages
242 The pandemic was top of mind for callers reaching the rebranded Family Support and Action Line. One Branch manager estimated that 90% of all calls received by the Branch during the first wave related to COVID. The accompanying chart shows the Ministry’s breakdown of COVID-related “intakes and questions” for this period.
Number of COVID-related “intakes and questions” the Inspections Branch received to July 31, 2020, by category.
| COVID category | Number of intakes and questions, up to July 31, 2020 |
|---|---|
| COVID-19 protocols | 1,247 |
| Visiting | 701 |
| Resident safety | 676 |
| Admissions/Discharge/Absences | 349 |
| Staffing | 213 |
| Infection Control | 187 |
| Screening | 158 |
| Total | 3,531 |
243 To help inspectors respond to public complaints and questions about COVID, Inspections Branch management prepared a “key messages” document. The messages were generally taken directly from another source with no additional context or interpretation. The first such document, from March 18, included the following “key messages”:
- Elderly individuals and those with underlying health conditions face a higher risk of COVID-19 complications.
- To ensure the safety of LTC residents, the Chief Medical Officer of Health has recently advised homes to only allow essential visitors until further notice.
- The Ministry is closely monitoring the situation and will provide update on this guidance around April 5, 2020.
- The Ministry expects and supports the LTCHs [long-term care homes] to act on the advice from Public Health and the Chief Medical Officer in all matters related to outbreaks and infection prevention and control.
- LTCH staff are required to be trained in infection prevention and control and to follow outbreak procedures according to best practices developed by Public Health.
- Essential visitors are people visiting residents who are very ill or require end-of-life care. No other visitors will be permitted to enter.
244 The Branch director sent the first set of key messages to inspectors on March 18, 2020, instructing that they be used to guide discussions with complainants. Inspectors were told to “not deviate from key messages or provide advice not already embedded in the attached document.” From that point, inspectors frequently relied on – and directly cited from – the key messages during calls with complainants. This was a substantial departure from the typical responsibilities of inspectors.
245 The Branch updated the key messages document regularly through the first wave of the pandemic as government directives and guidance changed. Over time, the document grew in length as it covered an increasing variety of topics.
246 Unfortunately, the Ministry’s new approach to intake and triage, combined with its failure to mobilize inspectors for an extended period during the first wave, led to a collapse in its ability to identify and act quickly on serious issues affecting residents in long-term care homes.
“Complete system breakdown”
247 As the Ministry began to experience the full impact of the pandemic and these process changes, the Inspections Branch struggled to cope. Its Director described the situation to us in stark terms: “It was a complete system breakdown. Like, it really, really was.”
248 Our investigators reviewed hundreds of complaint files to assess the work of the Branch during the first wave. While the experiences of individual complainants differed, our investigation found that the Ministry did not view COVID-related complaints to be high risk, nor did it properly consider how they should be triaged. It also did not have enough inspectors to handle the deluge of complaints, and there were serious issues with the documentation and communication practices within the Branch.
“Frustration, sadness and even anger”
249 During this time, many callers who reached out to the Ministry to raise critical concerns were met with little action or support, as inspectors simply parroted “key messages.”
250 Gemma experienced this situation firsthand. Both of her parents lived at the Mon Sheong Home for the Aged in Toronto.[103] On April 22, 2020, Gemma called the Family Support and Action Line and said her mother had passed away at the home from COVID, one of 22 COVID-related resident deaths there up to that point. We reviewed Ministry case notes for this and subsequent calls. According to these records, Gemma said the home was “severely short” on personal support workers (PSWs) and nurses, and had no PSWs during the night. She said residents “are not being fed, clean[ed] nor [given] medications.” Gemma asked the Ministry to “urgently send help” to the home and said she was worried about her father, who remained at the home and had also tested positive for COVID.
251 A Ministry inspector called Gemma on April 24. The inspector’s case note of the call said “no concerns had been identified regarding the staff from the home or the care they provided.” Gemma disagreed with this assessment, pleading with the inspector that the home needed help, adding: “We cannot let our parents just die there.” She reiterated that the home needed staff and the residents needed washing, cleaning, feeding, and hydration. According to the notes, the inspector “reassured” Gemma that people “may feel frustration, sadness and even anger in light of this situation.” The inspector talked about the Ministry’s COVID-19 Action Plan for the long-term care sector and provided general information about steps the Ministry was taking. Gemma was told that her concerns about the lack of testing and staffing “will be passed further.” The inspector then said that the complaint file would be closed. Based on the complaint records, no further action was taken regarding Gemma’s concerns and pleas for help.
Persistence doesn’t necessarily pay off
252 Peter also experienced considerable frustration as he reached out to the Ministry multiple times during the first wave.
253 His first contact occurred on April 6, 2020, when he alleged that the Altamont Care Community home where his mother lived was congested and not sending COVID-positive patients to hospital. Peter said this heightened the other residents’ risk of infection, and that he was very concerned for his mother’s health.
254 On April 8, a Ministry inspector called Peter and explained the home was working with the local public health unit, which understood the design of the home and the need to separate COVID-positive residents. According to the records we reviewed, the inspector noted that Peter had no concerns about the care that staff were providing to his mother, and that the inspector “de-escalated” the situation so that “no further action” was required. The inspector closed the file the same day, without recording any risk level associated with the complaint.
255 On April 14, Peter called again. He said he could not get information from the home about his mother amid the home’s COVID outbreak, but he had heard the home was grouping healthy and sick residents together.
256 On April 16, the inspector consulted with two managers, who advised him to share “key messages” with Peter. The inspector told Peter that public health was helping to separate the COVID-positive residents and provided him with information about the province’s Action Plan for long-term care. Again, the inspector closed the file without further action and without indicating a triage risk level.
257 On April 22, Peter made a third complaint. He said the home told him that his mother was very sick and had a low oxygen level, and he asked that she be sent to hospital. In reply, the home advised him his mother was “almost gone.” Peter said he then forcefully told the home to call an ambulance right away, which the home did. He did not receive an immediate response from the Ministry to this complaint.
258 On May 5, Peter made a fourth complaint – after his mother had died. (In total, 53 residents of Altamont died during the first wave, as well as one support worker.) He complained that the home wouldn’t release his mother’s medical records.
259 Two weeks later, on May 19, a Ministry inspector responded to Peter’s fourth complaint. Peter told the inspector he would be working with a lawyer to obtain his mother’s medical records. The inspector closed the file the same day without further action.
260 Meanwhile, Peter’s third complaint from April 22 remained open without any response from the Ministry. It was not until June 11 – 50 days after the complaint was made – that the Branch finally assigned it to the same inspector who had handled the May 19 complaint. According to the file notes, Peter became “very upset” when the inspector began asking about his mother, because she had since passed away from COVID. Peter said he had previously called the Ministry, and it had done “nothing.” He refused to give the inspector any more information. The inspector’s manager recommended an inspection. The file was assessed as a triage risk level of 3 (“Actual Harm” or “Actual Risk”).
261 On October 20, the Branch began its inspection, some six months after the complaint was filed and well outside of the timeframe for inspecting level 3 complaints (60 business days).
262 The inspector shared the results of the inspection with Peter on November 17. Peter was told the home was found in non-compliance because it had not referred his mother to a dietician despite her poor food intake. The Ministry did not find the home in non-compliance on other aspects of his complaint.
263 When our investigators asked the Ministry about its handling of Peter’s complaints, we were told inspectors were “overwhelmed” with inspections at that time, and it wasn’t clear that the Branch could have inspected Peter’s concern about sick and healthy residents living together, as the home’s inability to separate residents was due to its design. In any event, the Ministry was in no position to do an inspection in April 2020.
264 In a follow-up interview with my Office, the Ministry acknowledged that the Branch could have inspected the issue of neglect in Peter’s earlier complaints. Regarding the delay in responding to his third complaint, the Ministry said that during the first wave, they asked the inspectors to try to call complainants within 24 to 48 hours, even if just to acknowledge the complaint and arrange a later time to do the intake. However, sometimes this wasn’t possible. As one Ministry staffer put it: “We just didn’t have anybody. We had no resources.”
Oblivious to new risk
265 Although many aspects of its processes changed at the onset of the pandemic, the Inspections Branch made no modifications to how inspectors assessed the risk level posed by specific complaints. Peter’s interactions with the Branch, and its limited response to the concerns he raised, demonstrate how this affected complainants.
266 The Branch assigns a triage risk level to each “inspectable” complaint it receives, with level 4 being the highest. The chosen level reflects the risk that an alleged issue poses to residents and helps determine how the Branch will respond, and within what timeframe. In March 2020, the Ministry’s “COVID-19 Emergency Inspection Policy” directed that inspectors use the Branch’s existing triage risk level framework to assess the risk posed by each complaint. The triage risk levels and the rationale supporting them did not change when the pandemic began, and inspectors were not given any training or guidance on how COVID would factor into the existing system.
267 The Branch’s failure to consider the unique risks posed by COVID-19 is evident in the formal work plan it created when the pandemic began. From March 17 to 18, 2020, the Inspections Branch prepared a plan for the Deputy Minister’s office that set out the types of “high-risk scenarios” that inspectors would be monitoring during the pandemic. These included:
- Abuse of a resident that results in serious injury or death;
- Sexual abuse of a resident;
- [Departure] of a resident who gets hit by a car and results in serious injury or death;
- Suicide of resident;
- Bed-rail entrapment with death or injury;
- Choking where resident is hospitalized or dies; and
- Medication administration error where resident is hospitalized or dies.
268 While these are obviously serious issues, there was nothing identified that dealt specifically with the threat posed by COVID-19 in long-term care. There was no mention of large and deadly COVID outbreaks, inadequate infection prevention and control measures, failure to separate COVID-positive and healthy residents, or the potential risks of severe staffing shortages.
269 We spoke with senior Ministry officials who created and approved the plan, who told us that at the time the document was created, the impact that COVID would have in long-term care was not known. While it is understandable that the Ministry did not have direct prior experience, other worldwide and North American jurisdictions began experiencing large COVID outbreaks, resident deaths, and staff shortages in long-term care homes before the Branch prepared its plan.[104] If the Ministry had carefully considered the lessons learned from other jurisdictions, it might have been in a better position to predict what Ontario would likely experience.
270 The failure by the Inspections Branch to incorporate the specific risks posed by COVID into its triage system meant that when COVID-related complaints began coming in, inspectors did not categorize them as “high-risk.” In fact, none of the thousands of complaints related to COVID that the Ministry received during the first wave were triaged at the highest risk level (level 4). According to the triage system, an immediate inspection was not required for any complaints related to COVID during this period.
271 Even the next highest risk level (3+) was only applied to a few dozen complaints during the first wave. The information we received was incomplete and inconsistent, but one document we reviewed indicated that the Branch told senior Ministry officials that it received only three complaints between March 16 and April 30, 2020, that it considered to be level 3+. The Branch said those complaints involved “…abuse/neglect that resulted in death,” and it’s not clear if they related directly to the risks caused by COVID-19. Given the criteria set by the Ministry, it is not apparent why the Branch would have assessed these complaints at level 3+ – rather than level 4 – when they involved deaths of residents resulting from abuse and/or neglect at the home. Ministry policy classifies complaints of alleged abuse or neglect resulting in death as level 4, requiring immediate inspection.
272 Some first-wave complaints triaged at level 3+ after April 30 also suggested an extremely high level of risk, and it’s not clear why they were not considered level 4 issues. The Branch provided the following descriptions for five complaints categorized at this level:
- “…concerns regarding short staffing and neglect of care for mother […] and other residents due to COVID-19 outbreak / Pandemic. No trend.”
- “military observations of abuse, neglect, resident rights, medication not administered, nutritional care, staffing and leadership”
- “Complainant reporting she has no information on case: [personal support worker] fed resident […] on back resulting in death.”
- “Complainant has concerns about housekeeping, infected skin and wound care, resident being massively dehydrated, weight changes (loss), infection prevention and control measures.”
- “Complainant […] with concerns re neglect of resident […] resulting in his passing away.”
273 Each of these complaints potentially involved severe risk to residents. In two, the complainant alleged that the action or inaction of staff led to a resident’s death, yet none of these complaints were found to warrant the highest risk level.
274 The Inspections Branch made a critical error when it failed to consider how COVID would factor into the existing triage risk level system. Staff should have received concrete guidance and training on how the new reality of COVID-19 would affect the vital work of assessing the risk level of complaints. In future, it is imperative that the Ministry ensure that operational staff understand the risk posed by any new threat to the health and safety of long-term care residents and staff. It should provide clear guidance to Branch staff on how to assess that risk in practice, including through sharing practical examples of how to triage different issues related to the new threat. The goal of these examples should be to help inspectors apply their health care expertise and judgment in light of the new threat.
Recommendation 14
When faced with new or emerging threats in long-term care homes, such as a novel disease, the Ministry of Long-Term Care should provide inspectors and other staff with guidance and training on the risk that the threat poses to long-term care residents.
Recommendation 15
When new or emerging threats are active, the Ministry of Long-Term Care should adapt its triage risk levels to reflect the risk that the threat poses to long-term care residents.
Recommendation 16
The Ministry of Long-Term Care should provide staff with practical examples of what types of issues related to the new threat should be triaged at each risk level.
Missing risk level
275 In addition to finding many instances where Ministry inspectors chose a risk level that did not reflect the severity of the issue brought forward, our investigation also discovered numerous examples where inspectors failed to document a final triage risk level for the complaint. For instance, several of the complaints Peter made were missing this information.
276 During the first wave, a “job aid” in the Inspectors’ Handbook required inspectors to document triage risk level information when they closed a file. The requirement was more than a technicality, because if inspectors do not think about and document risk, they may be more likely to close files that contain high-risk issues without taking appropriate action.
277 In November 2021, the Branch deleted this job aid and requirement. The Ministry's list of policy changes said this was because it was “no longer applicable and information is in the policy-related guidance documents.” However, our investigation did not find any similar requirement in other Branch policies. Understanding and documenting the risk posed by each complaint is vital to ensuring that the Branch responds appropriately to alleged risk. The Ministry should ensure inspectors are required to state clearly what level of risk a complaint poses prior to deciding to close a file. It should explore the feasibility of creating a specific field in its documentation system that would require staff to enter this information before the file is closed.
Recommendation 17
The Ministry of Long-Term Care should ensure inspectors are required to record specifically what level of risk a complaint was found to pose, prior to closing the complaint file in the Ministry’s documentation system.
Too little, too late
278 Raheem had concerns about Altamont Care Community that were similar to Peter’s. He called the Family Support and Action Line on April 6, 2020 to complain that the same personal support workers were treating both COVID-positive and healthy residents. Both of Raheem’s parents lived in the home and he was worried for their health.
279 On April 8, a Ministry inspector called Raheem, who asked why the home was quarantining COVID-positive residents in rooms that also housed healthy residents. The inspector said they planned to make an inquiry with the home about its practices. According to the records we reviewed, the inspector emailed Toronto Public Health that day, asking to “quickly touch base” about a “few” complaints regarding Altamont. Of the 517 Ministry complaint files we reviewed, this was one of only two occasions where an inspector documented having contacted public health about a complaint.
280 On April 9, the inspector made a telephone inquiry with the home’s administrator and director of care, and wrote this note in the file:
Depending on the configuration of the resident room, some residents, with moving beds as far apart as possible, cannot be distanced 2 meters apart, however curtains are drawn to create an isolation area and all residents are treated in isolation. [The home] … considered moving residents to cohort them together, however there is the potential of cross contaminating when moving a resident as there could be the spreading of contact droplet around. [The director of care] stated that when one resident was positive in a ward room all residents have become positive, so currently there is no situation of a positive resident amongst uninfected residents in the same room. There is no separate place for the infected resident to be isolated.
281 On April 14, Raheem made a second complaint to the Family Support and Action Line, asking why COVID-positive residents could not be moved out of the home. The Branch added this new complaint to the already-open file, and the inspector called Raheem to relay the home’s “management strategies.” The inspector also wrote in the file that Toronto Public Health had not responded to her April 8 email, and that she had told her manager about her “concerns around the home not being able to separate residents.” Nevertheless, the inspector closed the file on both of Raheem’s complaints. She took no further action on the matter and did not document what risk level the issues posed to the home’s residents.
282 On May 12, Raheem called the Family Support and Action Line a third time. His father had contracted COVID at the home. Raheem had twice called an ambulance to the home, but the home turned each of them away. He said his father ultimately died of COVID at the home while severely dehydrated, and the home refused his request to release his father’s medical records. His mother had now contracted COVID at the home and was in hospital. According to the case notes, Raheem was “pleading for the Ministry to help this home.” In response to this complaint, a triage officer noted potential non-compliance in several areas, and documented the file as “Risk level 3; for inspection.”
283 On May 14, an inspector called Raheem, who said he was very upset with the home for not allowing his father to go to hospital before he died, and was considering legal action. The Branch proceeded with an inspection, which began on May 21, well within the Ministry’s timeframes. It found the home in non-compliance in multiple areas. However, the inspection report was not issued until July 29. The inspector apparently called Raheem to provide the results of the inspection, but the content of their conversation is not recorded in the Ministry’s file.
284 When we asked the Ministry about its handling of Raheem’s complaints, a manager told us the Branch could have done an onsite inspection of the earlier complaints, but it would have been “probably too late.” The manager said the situation was "so chaotic. It’s something I don’t ever want to experience again.”
285 In response to our questions about how the risk level 3 was assigned to this complaint, another manager acknowledged that the inability to separate residents and control spread of COVID created “horrific risk.” However, they said the Inspections Branch “had no answers” at the time, “didn’t know what to do,” and “didn’t have anybody trained.” They also noted that it’s not clear what the Branch could have inspected; the age and design of the home was a factor, and the home’s decision not to let the resident go to hospital was a doctor’s clinical decision that the Ministry could not inspect.
Narrow interpretation
286 Raheem’s interaction with the Inspections Branch mirrored Peter’s in many ways. Both cases also illustrate the narrow way in which the Inspections Branch interpreted its mandate during the first wave, even when resident safety was in serious jeopardy.
287 In each case, the inspection manager said the “capacity” and design of the long-term care home made it impossible to separate healthy and COVID-positive residents. The inspection manager told us the Ministry could not inspect that issue. We also heard from a few managers the Branch is unable to review homes’ decisions about whether or not to send residents to hospital.
288 It is not clear how the Ministry reached these determinations. Section 5 of the Long-Term Care Homes Act, 2007 (the legislation in effect at the time) stated that residents have the right to a safe and secure environment.[105] The “inspection protocol” document the Branch uses to inspect “Safe & Secure Home” issues says an “unsafe environment” could result from essentially anything that creates a risk of harm. This includes:
Any condition or circumstance, or influence surrounding and affecting the resident that may cause physical harm or risk of harm.[106]
289 With such a broad definition, the Branch would appear well positioned to inspect virtually any issue that results in risk to a resident. However, in the cases raised by Peter and Raheem, the Ministry did not inspect concerns about mixing COVID-positive residents with others; therefore, it had no way of knowing whether the capacity and design of the home was the only driver behind the spread of the virus. In Raheem’s case, the Ministry also did not gather any evidence to support its conclusion that it was actually a clinical decision to not send his father to hospital.
290 The Inspections Branch should not unduly limit its broad authority to inspect any complaint that alleges risk to a resident. If a complainant raises concerns about anything that potentially leaves a resident unsafe, abused or neglected, the Branch should use its legislative authority to inspect the issue, and, where necessary, take appropriate enforcement action.
Recommendation 18
The Ministry of Long-Term Care should amend the Inspections Branch’s policies and protocols to require inspectors to take a broad and inclusive approach to the complaint issues they can inspect, and to clearly state that the Branch has the authority to inspect any complaint that indicates a resident may be at risk of harm as a result of the home’s acts or omissions.
Missing notes
291 Raheem’s experience also demonstrates challenges the Ministry faced in keeping adequate records of calls and other communications related to complaints.
292 The Inspections Branch does not record its calls with complainants, but it has a policy requiring that inspectors make notes of their conversations with them. During our review of hundreds of Ministry complaint records, we found that inspectors consistently update the system after making calls to complainants. However, the quality of these records varied widely, and many notes provided no useful information about the purpose or content of a discussion.
293 In Raheem’s case, the inspector’s final call to him is reflected in an entry that says “Via telephone,” but there is no case note of the call itself. There is no information about what the inspector told Raheem, or his response.
294 We identified similar issues related to other matters. Calls to public health unit staff were poorly documented, and relevant information from support and monitoring calls to long-term care homes was usually not included in complaint files. This is problematic, as some managers recalled situations where the Branch relied on information from these calls when deciding how to respond to an issue. Without details about that information, it is impossible to assess the adequacy of the Branch’s response to specific complaints.
295 As a third party trying to use the available notes to piece together the story of a file, we found the widely varying quality of Branch case notes challenging. Poor case notes also impact the Branch’s ability to assess the work of its staff, prepare briefing notes about particular issues, and monitor trends.
296 A robust and credible inspection process requires detailed documentation. The Ministry should ensure that complaint files record all relevant activities, including the complete substance of communications with the complainant, the long-term care home, and third parties. Detailed documentation will also assist managers, who are responsible for auditing 5% of all inspection and inquiry files.
297 The Ministry should examine options to make audio recordings of calls to complainants, to help ensure it has a complete record of these conversations and further assist management when auditing files for quality and training purposes.
298 It should also ensure that any information relied on when deciding how to respond to a complaint, such as information from support and monitoring calls with long-term care homes, is clearly documented in the complaint file.
Recommendation 19
The Ministry of Long-Term Care should ensure that complaint files record the complete substance of all communications related to the file, including with the complainant, the long-term care home, and third parties.
Recommendation 20
The Ministry of Long-Term Care should examine options to audio record the Branch’s calls to complainants, and retain audio records in complaint files to ensure more accurate and complete records and assist management when auditing files for quality and training purposes.
Recommendation 21
The Ministry of Long-Term Care should ensure that any information relied on when deciding how to respond to a complaint is clearly documented in the complaint file.
“Miserable fail”
299 On May 18, 2020, Soren called the long-term care Family Support and Action Line to complain about the growing number of COVID cases at the Extendicare Guildwood home where his father lived. He noted that nurses were walking between areas that had COVID infections and those that did not. Soren said he feared everyone at the home would be infected by the end of that week.
300 On May 22, Soren called the Family Support and Action Line again, saying no one had called him back. He was anxious about the virus spreading and wanted to ensure the home was following the proper guidelines.
301 On May 28, Soren called a third time, saying it had been 10 days since his first call and no one had responded. He said 20 residents had died in 10 days, and he wanted information before removing his father from the home.
302 On June 4 – more than two weeks after Soren’s first complaint – a Ministry inspector called him, read him some “key messages,” and told him government and local public health officials were in regular contact with the home. The inspector said the local hospital had recently assessed the home’s infection prevention and control practices, and was following up to keep residents safe. Soren brought up many issues, including staff not always wearing gloves, delays in getting COVID test results, residents asking for water with staff nowhere to be seen, “horrific” staffing levels, and his own difficulty getting a COVID test for his father. The inspector acknowledged Soren’s frustration and fears, noted that these were difficult times, and then said they were closing the file. The notes indicate Soren chuckled, commented on the time it had taken the Ministry to respond, and said:
“I don’t think you should call [your service] ACTIONline.”
303 In closing the file, the inspector wrote that the “concern regarding infection control has been resolved.” He also noted that Soren was going to talk to the home about a test for his father, and would call the Ministry again if new concerns arose. The inspector’s closing comments did not identify the triage risk level for Soren’s complaints.
304 When we asked the Ministry about its handling of this file, we were told the Branch should have referred this case for inspection.
305 When we asked a Ministry official for thoughts on the time it took the Branch to respond to Soren, the official said: “It’s a miserable fail. It’s, yeah, these are the ones that break my heart.”
Ministry InAction
306 Although Ministry inspectors often returned complainants’ calls within a few days, some, like Soren, were left waiting weeks or even months for a response.
307 During the first wave, Ministry inspectors were expected to respond to complaints within two business days. We saw many cases in which they successfully met this timeframe, despite the huge number of files they were dealing with.
308 However, they didn’t always respond so quickly. It took the Branch more than two weeks to get back to Soren about a growing COVID outbreak that claimed the lives of 48 residents. He called the Family Support and Action Line three times over 10 days before anyone responded.
309 In Peter’s case, the Branch did not respond to his third complaint for 50 days, by which time his mother had died.
310 We also learned of a complainant who emailed the Premier on April 9, 2020, about not being able to get a COVID test for a sick parent at a long-term care home. The Premier’s Office forwarded the complainant’s email to the Inspections Branch within a week, but it took four further weeks for an inspector to call the complainant.
311 Serious complaints that were not related to COVID were also delayed during this time. It took more than two months for the Branch to return a call from a complainant who called in late March 2020 with one such concern. This complainant called three more times in an effort to obtain faster service. In another case, a long-term care resident called on April 24, 2020, alleging that she had been assaulted by another resident. This resident did not get a response from an inspector until June 16 – 53 days later.
312 Sometimes, complainants took matters into their own hands when the Branch didn’t call back. A woman called the Family Support and Action Line twice in May 2020 about issues related to a COVID outbreak at the Heron Terrace Long-Term Care Community home. When inspectors did not respond after a week, she directly emailed a senior Ministry official to share her disappointment in not having heard from a Branch inspector. The senior official forwarded this message to the Inspections Branch Director and told the Director he had spoken with the complainant himself. Eventually an inspector called her a few days later.
313 A Ministry staff person commented: “We should have been able to respond more rapidly to people … we’ve really let them down, you know, a lot of the public.”
314 We heard that sometimes the Ministry’s slow response was due to administrative confusion about whether anyone had called the complainant, and that the Branch has since modified its system so staff can more easily determine which complainants have not been contacted.
315 More often, though, slow response times were attributed to the Branch not having enough staff during this period. The large number of complaints and the lack of people to respond to them caused a backlog. Such a backlog can have serious consequences. The Branch doesn’t always have enough information to assess risk until it can conduct a full intake call with the complainant. It is vitally important that the Inspections Branch make contact with complainants promptly.
316 In February 2023, the government announced it had hired 193 additional long-term care inspection staff, including 156 inspectors. The Inspections Branch has also changed its policy to specify that it will respond to complaints in one business day. If the growth in Branch staffing is sustained, the new inspectors should be able to help the Ministry meet this goal. In order to monitor the Branch’s success in providing timely service, it should regularly audit files to assess whether it is consistently meeting the service standard of replying to complaints within one business day.
Recommendation 22
The Ministry of Long-Term Care should conduct regular audits of files to ensure that it is consistently meeting its service standard of responding to all complaints within one business day.
Co-ordination with public health units
317 Our review found little evidence that Ministry inspectors contacted other organizations, such as public health units, regarding issues raised by complaints. Among the 517 complaint files we reviewed, we only found two where an inspector documented contact with a public health unit. Raheem’s case was a notable exception – and in that case, Ministry records indicate that the public health unit did not respond to the inspector’s April 2020 email, and the inspector never followed up.
318 We asked the Ministry about its approach to raising issues with public health officials. We learned that there was little co-ordination or communication during the first wave of the pandemic. We were told of instances where inspectors tried unsuccessfully to communicate with their public health counterparts. Some public health officials asked for a letter of authorization before taking an inspector’s call. We heard that inspectors and their managers often did not know whom to contact when the pandemic began. This was a challenge, given that there are 34 different public health units, each with separate contacts.
319 Ministry officials initially told us there was no policy or process covering how and when inspectors should contact public health units or other third parties about complaints. However, communication slowly improved through subsequent COVID waves. In April 2022, the Ministry told us it is working on “proposed frameworks” for the sharing of information between the Ministry and public health units.
320 Given the importance of information sharing, the Ministry should introduce a clear policy specifying the situations in which Ministry inspectors should reach out to public health units regarding complaints. This policy should also indicate what information is to be shared with public health units.
Recommendation 23
The Ministry of Long-Term Care should introduce a policy specifying the situations in which Ministry inspectors should reach out to public health units regarding complaints and the information that may be shared with public health units in certain circumstances.
321 Even if Ministry inspectors had managed to contact relevant public health units regularly about complaints during the first wave, it is not clear how the units would have responded. The province’s current pandemic plan – the 2013 Ontario Health Plan for an Influenza Pandemic – does not specify what role public health units should play in the context of long-term care homes during a pandemic, or how they should co-ordinate with the Ministry of Long-Term Care. While previous iterations of the plan had a specific chapter for long-term care homes, the government removed this information for the 2013 version. It would have been useful during the early and chaotic days of the first COVID wave to have clear roles, responsibilities, and co-ordination agreements in advance.
322 The Ministry of Long-Term Care should work with public health units to clarify the units’ role regarding long-term care home inspections during any future public health emergency. It should proactively educate the public health units about matters relevant to the role of the Inspections Branch, including providing examples of which complaints should be referred to the Branch.
Recommendation 24
The Ministry of Long-Term Care should work with public health units to clarify the public health units’ role regarding long-term care home inspections during any future public health emergency.
Recommendation 25
The Ministry of Long-Term Care should proactively educate public health units about the role of the Inspections Branch, including providing examples of which complaints should be referred to the Branch.
Limits of “key messages” and “support”
323 When Soren called the Family Support and Action Line, he clearly wished to complain about specific issues in his father’s long-term care home. Instead of having his concerns flagged for inspection, he received “key messages” from the inspector and the complaint was closed.
324 Soren’s experience was not unique. Based on the files we reviewed, the Inspections Branch closed many of the complaints it received during the first wave with just a call back to the complainant and no further action.
325 We heard that this occurred because a large proportion of the calls involved questions, concerns or complaints about government directives in general, and that in such cases, the Ministry inspectors could do little more than provide the approved key messages. One Inspection Manager told us that in those cases, inspectors would provide information, explain to callers that their issues weren’t the type that the Branch could inspect, and close the file.
326 In the file notes we reviewed, it is not always easy to distinguish where key messages were an appropriate response to the complaint, and where an inspection could have occurred. The Ministry’s own system does not differentiate between true “complaints” requiring triage and possible inspection, and questions or information requests where it may be appropriate to provide general information to the caller. This confusion was likely compounded by the complaint line’s change in name from ACTIONLine to “Family Support and Action Line.”
327 While there was substantial value during the first wave in having a government resource available to answer questions related to long-term care, tasking Ministry inspectors with this role was confusing for all involved. Complainants who were seeking an inspection of their concerns received “support” instead, and inspectors whose normal role was to conduct compliance inspections were asked to support callers through a difficult crisis.
328 The phone line for making complaints about long-term care is still called the Family Support and Action Line. Given the role of the Inspections Branch, the Ministry should remove “support” from the name of its complaints line and adopt a name reflecting the true purpose of the Inspections Branch.
Recommendation 26
The Ministry of Long-Term Care should remove “support” from the name of its complaints line and adopt a name that accurately reflects that the purpose of the line is to enable individuals to file complaints that the Ministry can review and act upon.
329 We reviewed numerous files where complainants like Soren raised specific issues that appeared, on the surface, to pose a serious risk to residents’ health and safety, only to have inspectors close them after providing “key messages.” It was often unclear why key messages were considered to be an appropriate response to the issues raised. The Ministry should have clear criteria distinguishing between specific complaints and more general requests. It should direct staff to treat all files that are not clearly questions or requests for information as complaints requiring triage and inspection. If a file is determined to be a question or a request for information rather than a complaint, this should be specifically documented, and statistics on these types of cases should be tracked separately. This would assist the Ministry in differentiating between complaints, questions, and requests for information in its files, and also ensure that inspection staff have actively considered whether an individual has raised a question, information request, or a complaint.
Recommendation 27
The Ministry of Long-Term Care should establish criteria for distinguishing between complaints, questions, and requests for information, and direct staff to treat all files that are not clearly questions or requests for information as complaints requiring triage and inspection.
Recommendation 28
The Ministry of Long-Term Care should direct staff to document whether a file is a question, request for information or a complaint.
Recommendation 29
The Ministry of Long-Term Care should keep separate statistics for complaints and for requests for information.
Fast-tracked inquiries
330 Even when the Inspections Branch is operating normally, it has the option of making an “inquiry” with long-term care homes – rather than conducting an inspection – for complaints that are unresolved but “low risk.” It follows a similar practice when dealing with critical incident reports. The Branch categorized more than 8,000 files as inquiries in 2019. Typically, complaints are categorized as warranting Ministry inquiries when they are triaged as risk level 1 or 2. The purpose of an inquiry is to ensure the home is complying with the legislation, and it does not result in a formal report that is made available to the public. This process is contemplated by the long-term care legislation, which states that the Ministry must “conduct an inspection or make inquiries” in certain cases.[107] All files that do not result in an inspection are “inquiry files,” even if the inspector takes no action.
Typical inquiry process
331 The Ministry has established a written process for files that are treated as inquiries. The inspector only proceeds with an inquiry if the issue remains unresolved, low-risk, and not subject to a recent inspection. For complaint files, the Branch gives the complainant the option of trying to resolve the issue directly with the home first. If the complainant agrees to do so, the Branch closes its file and does not make an inquiry.
332 Once it is determined that an inquiry will be made, the inspector prepares an inquiry plan and determines whether the inquiry will occur “on site” (at the long-term care home) or “off site.” By default, inquiries are done off site and are supposed to occur within 90 business days.
333 When conducting an off-site inquiry into a complaint, the inspector interviews staff from the home using pre-established questions as a guide. If needed, the inspector can ask the home for relevant documents, such as care plans or meeting minutes.
334 The inspector then determines what steps should be taken next. In most cases, they close the file or escalate it to an inspection. Once the inquiry process is finished, the inspector is expected to contact the complainant within two business days to discuss the results. In cases where inspectors find low-risk non-compliance, they are expected to inform complainants.
Inquiries during COVID
335 Although inquiries were common before the pandemic, the Branch used this process in unexpected and unprecedented ways during the first wave of the pandemic.
336 Beginning around March 20, 2020, an internal change to the Ministry’s process meant that all COVID-related cases were initially labelled as “inquiries”. This was not because every file was considered low-risk. Rather, it was an administrative method for transferring the file to inspectors, who had become responsible for conducting complaint intakes.
337 Notwithstanding the “inquiry” label, Ministry inspectors were not supposed to be making inquiries with long-term care homes about individual files. The Branch Director provided this direction to inspectors on March 18, 2020. Service area office managers reiterated the message.
338 While some inspectors we spoke with recalled making inquiries during this period, we saw many examples in files where they told complainants they were unable to call a home due to the moratorium on inquiries. In a file we reviewed from March 27, 2020, an inspector wrote “the Ministry is not conducting inquiries at this time, therefore, the inspector cannot inquire specifically about this resident.” In another case, an inspector wrote on May 4 that he told a complainant the Ministry had temporarily “suspended the inquiry or inspection due to the COVID-19 situation.”
339 However, we also heard that some inspectors asked about complainants’ individual concerns during support and monitoring calls. Examples from complaint files we reviewed from late March 2020 included inspectors making inquiries about whether an essential visitor was warranted for a particular resident, a home reportedly continuing to allow non-essential visitors, a home allegedly allowing short-stay absences after the government had prohibited them, and a home allegedly refusing to allow a resident to return after a leave of absence. A number of “inquiries” also occurred in April 2020.
340 We also reviewed Ministry emails relating to cases where Branch managers specifically asked inspectors to make inquiries with homes about issues, despite the general direction not to make them.
341 The continuation of inquiries by some inspectors during the first wave meant certain inquiries on low-risk issues happened much faster than inspections of high-risk complaints. Many of the inquiries that inspectors made during the first wave happened within a day or two of the Inspections Branch receiving the complaint – sometimes even the same day. Meanwhile, the Branch did not act on some high-risk issues that needed inspection for weeks or even months due to the pause in on-site inspections and the resulting backlog. This inverted prioritization is contrary to Ministry policy, which calls for inspections on high-risk issues to happen much faster than inquiries on low-risk issues.
The stakes should be low
342 Inquiries are only supposed to be used for low-risk files. However, during the pandemic’s first wave, the Inspections Branch conducted inquiries on some COVID-related complaints that appeared to present serious risk to residents. In Raheem’s case, a Ministry inspector made an inquiry with a home to ask about the spread of COVID and the home’s ability to separate infected and healthy residents. The inspector learned the home could not do so and that infected residents were readily spreading the virus to others in the same room. The inspector appeared concerned and alerted an inspection manager, but then closed the file without further action.
343 In another case from April 2020, an inspector made an inquiry about an alleged assault of a resident by a staff member, which resulted in the resident being taken to hospital. We do not know why this was initially categorized as an inquiry, but it was likely because inspections were not occurring at that time, and calling the home was the only way the inspector could look into this serious allegation.[108]
344 The Ministry should ensure that inspectors assess all files in accordance with the triage risk level criteria in the Branch’s policy and only use the inquiry process for issues that present little or no risk to residents.
Recommendation 30
The Ministry of Long-Term Care should ensure that the inquiry process is only relied on for issues that genuinely present little or no risk to long-term care residents. Issues that present greater risk should be inspected, as required by Ministry policy.
345 In assessing risk levels for issues that affect an individual resident, the Branch only assesses whether that same issue was reported for the resident three times in the previous six months. This means the Ministry is not looking to see whether it has received similar complaints related to other residents. For operational or environmental issues affecting the home, the Ministry considers an issue that has been reported three times in six months to be a “trend.” While that may be an appropriate threshold for some issues, others can be cyclical and/or recur over longer periods (e.g., seasonal temperatures or disease outbreaks). In determining that an issue presents a low risk, the Ministry should ensure that it has done a meaningful trends analysis that takes into account the many ways that an issue may manifest in a home. For instance, if the same concern has arisen with multiple residents at the same home over a short period of time, it could represent a trend worthy of inspection.
346 The Branch can only be confident that an issue is low-risk, and thus appropriate for an inquiry rather than an inspection, if it has conducted sufficient research to confirm that it is not part of a broader trend in the home. The Ministry should enhance its process for assessing trends to ensure that it takes into account situations where the same issue has been raised in connection with different residents of the same home. It should also ensure that inspectors have flexibility to assess trends over longer periods.
Recommendation 31
The Ministry of Long-Term Care should enhance its process for assessing trends to ensure that it takes into account situations where the same issue has been raised in connection with different residents of the same home.
Recommendation 32
The Ministry of Long-Term Care should also ensure that inspectors have flexibility to assess trends over longer periods in instances where the issue may arise seasonally.
347 Inspections Branch management should play a vital role in ensuring that only low-risk issues are handled through the inquiry process. Our investigation found that managers do not always review or approve files that are closed as inquiries. That means there is no check to ensure that nothing high-risk is overlooked.
348 This occurred in Soren’s case. He reported serious concerns about the home his father lived in, including staff not wearing gloves, delayed test results, “horrific” staffing levels, and more. The inspector treated the file as an inquiry file and closed it, even though no inquiries were made. After reading over the reports for that case, a senior Ministry official told us: “Anything like this should never be an inquiry [file].”
349 On paper, the Branch has an audit process that could catch some wrongly-closed inquiry files after the fact. The Branch’s policies say managers should review 5% of inspection files and 5% of all inquiry files. For inquiry files, audits should ensure the decision to close the file without an inspection was appropriate, and that the inspector contacted the complainant before and after the inquiry. At least one inspection manager we spoke to was unaware of the audit requirement for inquiries; this manager told us the Branch only audits files that result in an inspection.
350 Given the serious implications of misclassifying complaint issues, the Ministry must do more to ensure that anything closed as an inquiry file is genuinely low-risk. It should enhance its current audit program to ensure that all managers are aware of and comply with the requirement to audit inquiry files. It should also increase management oversight for closing inquiry files – for instance, by requiring managers to approve such files before they are closed, or to audit a larger percentage of closed files.
Recommendation 33
The Ministry of Long-Term Care should take steps to ensure Branch managers are aware of and comply with the requirement to audit inquiry files.
Recommendation 34
The Ministry of Long-Term Care should increase management oversight for closing inquiry files. For instance, the Ministry could increase the percentage of inquiry files that managers must audit, or it may require a manager’s approval for closing an inquiry file.
351 In cases where an instance of low-risk non-compliance is found during the course of an inquiry, Ministry policy provides that the inspector can document it without conducting an inspection or issuing an inspection report. As a result, low-risk non-compliance identified during inquiries is not included in a home’s compliance history and does not factor into Branch decisions about future enforcement actions. Several managers and inspectors we spoke with raised concerns about this approach. In the past, inspectors were required to at least inform homes about non-compliance identified during an inquiry. However, since late 2021, they have been specifically instructed not to do so.
352 The implications of non-compliance identified during inquiries should be minimal, since only low-risk issues are subject to inquiries. However, failing to inform homes about these findings and not including them in their compliance history is inconsistent with the Ministry’s oversight role and the intent of the legislation. The Ministry should direct inspectors to inform homes of any instances of non-compliance identified during inquiries and ensure they are appropriately documented and considered as part of the home’s compliance history.
Recommendation 35
The Ministry of Long-Term Care should direct inspectors to inform homes of any instances of non-compliance identified during inquiries and ensure they are appropriately documented and considered as part of the home’s compliance history.
The complaints that were never made
353 The pandemic’s first wave understandably resulted in many more complaints than normal to the Inspections Branch. However, our investigation revealed that many of those who were most directly affected – long-term care residents themselves –found it difficult to raise their concerns, due to structural barriers.
354 Many residents spent long periods confined to their rooms. Those without their own phone or Internet connection were cut off from the complaint process. Others who had such access were deprived of the assistance they required to make use of it, thanks to visitor restrictions and staff shortages.
355 Many residents entrust their concerns about their living conditions to family members, loved ones, privately paid companions, and personal support workers, who in turn relay them to the Ministry. During the first wave, resident access to these individuals was substantially limited.[109] Moreover, the residents’ councils[110] at many homes stopped functioning during the first wave because neither the homes nor the Ministry considered them to be essential, even though they typically play a key role in amplifying residents’ concerns.
356 In addition, the Ministry stopped conducting on-site inspections for more than seven weeks, meaning residents had no opportunities to share their concerns in person with an inspector or for the inspector to identify issues through observation.
357 Long-term care residents must always have a practical way to voice concerns about their safety and the care they are receiving. During any future public health emergency, the Ministry should do everything it reasonably can to ensure residents can access all of the usual complaint avenues to raise issues about their safety and care. That includes ensuring that they have a way to communicate directly with the Ministry during outbreaks and other emergencies.
Recommendation 36
The Ministry of Long-Term Care should ensure that long-term care residents can always meaningfully access complaint avenues during disease outbreaks and other emergencies.
358 Our investigators also heard concerns that would-be whistleblowers did not feel safe contacting the Inspections Branch during the early days of the pandemic.
359 The Long-Term Care Homes Act, 2007 and its successor, the Fixing Long-Term Care Act, 2021, are meant to protect long-term care home staff, residents, their family members and others from reprisal when they file complaints with certain organizations. Specifically, the legislation forbids any person from retaliating (or threatening to retaliate) against anyone who gives information to a Ministry inspector, Inspections Branch Director, or as part of a proceeding under the long-term care legislation or Coroners Act.[111] It also forbids long-term care homes and staff from attempting to discourage anyone from raising concerns. It is an offence to retaliate against someone for making a complaint, or to attempt to stop someone from making a complaint.
360 Our investigation identified a small number of staff complaints to the Inspections Branch during the first wave. In April 2020, a long term care home staff member called a Ministry inspector directly to say the home had no staff left to feed or care for residents. The inspector asked the person to call the Family Support and Action Line to make a complaint. The staff member refused and hung up. Nonetheless, this information rapidly made its way to senior Inspections Branch management, who became involved in calls to the home and its operator.
361 In our interviews with Ministry inspectors, they told us about other first-wave staff complaints, including:
- An anonymous staff member alleging a home was not following screening directives;
- Agency staff raising concerns about a home’s infection prevention and control measures and screening protocols; and
- Staff concerned that a home had told them not to wear masks.
362 We received limited information about how the Ministry responded to these complaints. We were told that the inspector in the first case called the whistleblower, explained the relevant protections in the legislation, and invited the staff member to call again if they experienced retaliation. We were also told generally that for concerns about COVID protocols, inspectors would call the long-term care staff and explain the government’s directives.
363 Some whistleblowers also contacted our Office, rather than the Ministry, indicating they did not feel they would be protected if they made a complaint to a long-term care home or the Ministry directly. One staff member at a long-term care home told us in June 2020 that residents were declining due to being confined to their rooms for more than two months without mental stimulation. This worker said the home was understaffed and didn’t have sufficient personal protective equipment. They also feared loss of employment if they flagged their concerns to the home. Our staff provided this individual with referrals to address these concerns.
364 We heard similar concerns from stakeholders, who indicated that many long-term care workers had seen colleagues fired for raising concerns, and that many feel the Ministry was not able to effectively prevent such retaliation.
365 During the early weeks of the first COVID wave, in the absences of Ministry inspectors and most outside visitors, those working in long-term care homes were in the best position to observe the actual conditions within. We will never know how many staff could have brought serious issues to the Ministry of Long-Term Care’s attention, but did not feel safe in doing so.
366 This concern has been recognized by other oversight bodies, and both the Patient Ombudsman and the Long-Term Care COVID-19 Commission have called on the government to improve the protection it affords to whistleblowers. While there are some protections in the Act, including for evidence given in a proceeding,[112] our investigation provides further evidence that many staff are afraid to raise concerns about long-term care homes. The Ministry should ensure that the whistleblower protections are as robust as possible, and should work with the Government of Ontario to expand them to clearly cover any complaint raised about a long-term care home to any applicable body, including the Ministry of Long-Term Care, the Ministry of Labour,[113] public health units, the Patient Ombudsman, our Office, and the homes themselves. Specifically, the Government should utilize the Lieutenant Governor in Council’s (this means Cabinet with the formal approval of the Lieutenant Governor) regulation power under section 41(2)(s) of the Fixing Long-Term Care Act, 2021 to amend section 117 of O. Reg. 246/22 to include additional avenues of complaint that attract whistleblower protection.
Recommendation 37
The Government of Ontario should revise the whistleblowing protections in section 117 of O. Reg. 246/22 under the Fixing Long-Term Care Act, 2021, so that its protections clearly apply to concerns raised about a long-term care home to any applicable body, including the Ministry of Long-Term Care, public health units, the Patient Ombudsman, the Office of the Ontario Ombudsman, and the long-term care homes themselves.
367 The Inspections Branch should also take steps to increase confidence among long-term care home staff and others in its ability to effectively respond to complaints from whistleblowers. This should include establishing procedures to protect whistleblowers’ identities and their files, and publishing information about these processes and the relevant legislation on its website.
Recommendation 38
The Ministry of Long-Term Care should develop a written process to better protect whistleblowers’ identity, including establishing procedures to protect whistleblower files, and it should publish information about these processes and the relevant legislation on its website.
368 The Inspections Branch is also tasked with inspecting allegations that homes have contravened the whistleblowing protections in the Act. The Ministry should enhance its process for dealing with allegations of retaliation. At present, Branch policy requires positive proof of retaliation from two of three sources (i.e., interviews, observations and reviewing records), which can be difficult to obtain. This is because retaliation is treated the same as complaints about other issues, which all require evidence from two of three sources to result in a finding of non-compliance.
369 The unique circumstances of retaliation complaints and the possible sources of evidence require an individualized approach. The Branch should amend its policy for cases of alleged retaliation to provide inspectors with greater flexibility, including by not requiring two sources of evidence.
Recommendation 39
The Ministry of Long-Term Care should amend its policy regarding cases of alleged retaliation to provide inspectors with greater flexibility regarding evidence that would support a finding of retaliation.
Critical Incidents
370 Along with responding to specific complaints, the Branch also conducts inspections in response to “critical incident reports” received directly from long-term care homes. Critical incidents are a key driver of Ministry inspections. Prior to the pandemic almost half (49%) of them stemmed from a critical incident report. This leaves the Ministry’s inspections system heavily reliant on long-term care homes reporting serious issues themselves.
371 Long-term care homes are required by regulation to report “critical incidents” to the Ministry.[114] With respect to infectious diseases, including COVID-19, homes must “immediately” report an outbreak in as much detail as is possible in the circumstances. If the Ministry learns that a home didn’t report a critical incident as required by law, the Inspections Branch can inspect that omission.
372 A senior Inspections Branch manager told us that before the pandemic, any infectious disease outbreak reported at a long-term care home was typically “monitored” by the Ministry until the local public health unit advised that the outbreak was over. The Branch then closed the critical incident file. We were told that an inspection would occur during the monitoring period if “needed”, but it is not clear what criteria were used in making this determination.
373 Based on data we reviewed, prior to the pandemic it was rare for the Ministry to inspect critical incident reports of disease outbreak. This is consistent with data analyzed by the Auditor General, who found that, from 2016 to 2019, the Ministry only conducted inspections in 6% of reported cases of acute respiratory infection outbreak.[115] In a further 4% of cases, the Ministry made a phone inquiry with the home. In 90% of cases involving disease outbreaks, the Ministry did nothing and then closed the file.
Critical incidents during the first wave
374 The Ministry’s approach to critical incident reports about infectious disease did not change much during the first wave of COVID-19. Long-term care homes were expected to make reports to the Ministry for any COVID outbreaks and related deaths. Early in the pandemic, homes had to improvise when reporting their outbreaks, as the reporting system did not have an option for “COVID” (it took until September 2020 for this to be added).
375 Our investigation found one instance in which the Ministry followed up on a home’s failure to file a timely critical incident report related to a COVID outbreak: It found the Altamont Care Community home submitted a report more than two months late. The inspectors gave the home a “written notification” for this delay, which is the least severe enforcement action possible, and one that doesn’t require any follow-up action from the Branch.
376 At other times, the Branch instead “reminded” homes to submit a critical incident report for a COVID outbreak, rather than taking enforcement action. We heard the Branch often took a similar approach if homes failed to report COVID-related deaths, which would typically be considered critical incidents, because the deaths were sudden or unexpected.
377 The Ministry did not conduct any inspections of outbreak-related critical incidents until June 2020, when it conducted three. When we asked about these low numbers, Branch officials described doing other things with the critical incident reports that weren’t formal inspections. One inspection manager said inspectors would call the affected home to ask if the local public health unit had confirmed the outbreak, obtain more information, and offer assistance. Others described making daily follow-up or monitoring calls to the home until the outbreak was over. Still others indicated that these conversations occurred during the official “support and monitoring” calls conducted by inspectors.
Preparing for future pandemics
378 In January 2021, the Branch introduced two new policies that affect how inspectors approach COVID-related critical incidents. When a critical incident report is received regarding a disease outbreak, inspectors must assess whether any infection prevention and control (IPAC) assessments occurred at the home in the past six months. That includes any IPAC assessment by the home itself, by a third party, or by a Ministry inspector.
379 If there has been no assessment in the past six months, the Branch assigns the case a risk level 4, and it is immediately inspected.
380 This approach is an improvement on how the Branch responded to critical incidents about COVID outbreaks in the first wave. However, even this new policy has gaps. A long-term care home can avoid immediate inspection if it has done an IPAC assessment on itself in the previous six months, regardless of the rigour or results of that assessment. Given that there are no checks and balances to ensure the quality of such self-assessments, the Ministry should not rely on them when deciding whether an immediate inspection is warranted in response to a critical incident report of disease outbreak.
Recommendation 40
The Ministry of Long-Term Care should not take into account any prior self-assessments conducted by a long-term care home when deciding whether an immediate inspection is warranted in response to a COVID-related critical incident report.
381 Although the Ministry has already implemented important policy changes for outbreak-related critical incidents, a broader rethinking of the critical incident reporting process would make it more responsive now and during future emergencies. During a crisis, the things that pose the most serious risk to residents can change. In addition to the existing list of events in the regulations that must be reported as critical incidents, the government should add a catchall category covering any situations when residents are at risk of serious harm, whatever the cause. During a pandemic emergency, this would require homes to report dangerously low staffing or PPE shortages as critical incidents. Such a process could avoid the need for a separate (and voluntary) support and monitoring process to collect this kind of information.
Recommendation 41
The Government of Ontario should amend the regulations under the Fixing Long-Term Care Act, 2021 to include a category covering situations where residents are at risk of serious harm, whatever the cause, in the list of circumstances requiring long-term care homes to file critical incident reports with the Ministry of Long-Term Care.
First-wave Inspections
382 When inspections eventually resumed in May 2020, the Inspections Branch had to prioritize which ones to do first. As the Director explained to us, it wasn’t “business as usual,” and some service area offices were dealing with many homes in outbreak.
383 On May 7, 2020, the Deputy Minister of Long-Term Care asked the Inspections Branch to start inspections at all long-term care homes that had been deemed at highest risk from COVID by one of the government’s inter-ministerial advisory tables. The Deputy Minister said the Ministry needed a “sense of what is actually happening on the ground” at those homes to help it decide on how to respond. The Deputy Minister asked the Branch to organize these inspections for the next day (May 8) and/or the following Monday.
384 The following day, the Inspections Branch Director asked senior managers to look for complaints regarding homes that were categorized at the highest or second-highest level of risk. The Branch director also asked them to find critical incident reports related to abuse or neglect at homes where they felt the risk was high. In response, senior Branch managers prepared schedules showing which inspections they planned to prioritize through the rest of May.
385 This approach was a notable departure for the Inspections Branch. Its normal practice before the pandemic was to rely on its own internal triage risk level system to determine how quickly an inspection should happen. Its system is based on the risk of harm that the identified issue poses to residents. In contrast, the advisory table’s risk assessment model was about the risk that COVID – and only COVID – posed to the home; it didn’t necessarily take account of other issues.
386 The Inspections Branch was able to start some inspections of the highest-risk homes very quickly, although it took several weeks to get to others. One of the biggest challenges was that the highest-risk homes were not evenly distributed across the province. As of May 8, 14 of the 30 high-risk homes were in the Toronto area and eight were in Central East. The other five service area offices had a combined total of eight homes at this risk level.
387 By May 21 – about two weeks after the resumption of inspections – the Branch was still struggling to get inspectors into all of the high-risk homes. It had completed only five inspections of the 30 homes in this category, and started inspections at 11 others. Yet as of the same date, it had started inspections at some medium-risk homes in hard-hit areas, as well as at the lowest-risk homes outside the Toronto area. The Branch director explained to us that some service area offices – those that didn’t have a large number of high-risk homes – had been able to resume regular inspection activities at homes that were not in outbreak.
388 About a week later (May 27), the number of high-risk homes had decreased to 21, as some emerged from their outbreaks, but the Branch was still straining to get inspectors into them. Only three inspections of the highest-risk homes were complete and nine were in progress.[116] As of June 12, there was still one high-risk home the Branch hadn’t been able to visit.
Staffing struggles
389 Our investigation determined that the shortage of investigators was caused in part by a decision the Branch’s pre-pandemic practice of leaving inspector positions vacant, and its initial decision to rely on volunteers when on-site inspections resumed in May 2020.
390 As the first wave of the pandemic began, on paper, the Branch had a complement of 171 inspector positions. However, only 152 were filled. Only 54 of those inspectors initially agreed to go on-site to complete inspections when they resumed. Only four were based in Toronto, where almost half of the high-risk homes were located. Hamilton, which was also hard hit by outbreaks, had only three inspectors to conduct on-site work. In an interview with our investigators, the Inspections Branch Director said there were not “even nearly enough” inspectors during the first wave to do desperately needed inspections, especially in the Toronto area. The Deputy Minister expressed similar concerns in his June 10, 2020 email to the Treasury Board. A different Ministry official put it to us bluntly:
There was nobody [willing] to inspect…We were in a crisis situation and we were making decisions based on what we were facing here. We were just, you know, in a very bad situation.
391 We were told that on April 29, the Ministry only asked volunteers to do on-site inspections, in an effort to get inspectors back in the field quicker in the face of their union’s continued concerns. On May 8, the Ministry asked inspectors who had not volunteered – but who had not sought an accommodation – to begin inspecting homes as well. But it was still short-handed, because a large number of inspectors (76 of 152) sought and received accommodation relating to medical or other restrictions. Even by July 2020, Toronto and Hamilton only had four inspectors each who were willing to enter homes experiencing COVID outbreaks. We were told that inspectors from other regions were brought in to assist.
392 On August 4, 2020, senior Branch managers circulated a formal strategy for scheduling inspectors. It called for the Branch to continue to first deploy inspectors who were willing to inspect homes experiencing COVID outbreaks, but it also contemplated scheduling those who had no restrictions preventing them from conducting on-site inspections. The Branch also determined that inspectors who had accommodation for non-medical reasons would be sent to homes not in COVID outbreak, while those who had accommodation for medical reasons would be given work appropriate to their requirements.
393 It took months for inspector staffing issues to improve, and this affected the effectiveness of the Branch in ensuing waves of the pandemic. The shortage had significant and enduring effects on the Branch’s ability to carry out its mandate.
394 The inspector shortage, combined with the earlier pause on inspections, resulted in a growing backlog of complaints and incomplete inspections through much of the first wave. At the end of February 2020, the Branch had 395 outstanding inspections. By the end of June 2020, that number had more than tripled, to 1,211.
395 The Branch prepared a slide deck in September 2020 that showed the impact of the backlog. At that time, it estimated it would take each of the available inspectors 272 days to work through all the outstanding inspections. This did not account for new inspections that would pile up in the meantime. Under the Ministry’s guidelines, depending on the priority level assigned to a complaint or critical incident, an inspection should start immediately, or within 30 to 60 business days (there is no timeframe for completing the inspection). The Branch had no chance of meeting its inspection timelines for a huge number of complaints and critical incidents with such a backlog. This was further complicated by the fact that the outstanding inspections were not distributed evenly across the province. While some regions made significant progress over the summer of 2020, Toronto’s backlog continued to increase. By October 2020, the Toronto office had more than 300 outstanding inspections.
396 The Branch still managed to inspect some high-risk issues fairly quickly once inspections resumed. But some files took a long time – many months in some cases. A February 2020 complaint about a resident who fell at the Yee Hong Centre Mississauga home was categorized at risk level 3. The required inspection should have started by mid-May 2020, but inspectors did not begin their work until late June 2020, about six weeks beyond the 60-day standard. In another case from May 2020, a woman complained about her husband’s death of unknown causes at Bradford Valley Care Community home. The Branch assessed the case as a risk level 3, with potential non-compliance around infection prevention and control, but the inspection started in mid-September, about a month outside the Ministry’s expected timeframe.
397 Because the Branch does not consistently track when inspections begin, it is hard to know how often it met the timelines set out in Ministry guidelines. Some staff we spoke with were not even sure how to interpret the guidelines, and whether they required that an inspection begin or end within a specified period. However, when speaking with our Office in late 2020, the manager of the Hamilton service area office told us it had about 100 “past due” inspections at that time, and that the London area had loaned them four inspectors to help work through the backlog. We also heard that in Toronto, 227 inspection files were overdue as of November 2020.
398 One of the long-term care residents we spoke to bluntly described her frustration with the timeliness of the Branch’s inspections:
Why should the resident or the family use the Ministry phone number? Because nothing is going to happen […] Residents and families feel, why bother making complaints if nothing happens? If they make complaints, it takes forever for the inspector to come back and look into the complaint.
399 The Ministry establishes inspection timelines to help ensure that all concerns are addressed expeditiously and that the most serious are inspected first. It should consistently track when inspections begin so it can assess whether it is meeting relevant timelines and take any necessary remedial action. It should also provide staff with clarification on how to interpret the inspection timelines.
Recommendation 42
The Ministry of Long-Term Care should consistently track when inspections begin, monitor whether it is meeting its inspection timelines, and take any necessary remedial action.
Recommendation 43
The Ministry of Long-Term Care should also provide staff with clarification on how to interpret the inspection timelines.
400 Even into 2021, the Ministry struggled to deal with the backlog. We were told the Branch did 2,046 inspections between January 1, 2021 and January 31, 2022 (a period of 13 months) – 157 inspections per month on average, far below the Branch’s 2019 monthly average of 240.
401 As of February 2022, the number of inspectors had decreased to 148. Of these, only 116 were able to conduct on-site inspections. In February 2023, the Ministry announced it had hired 193 long-term care inspection staff, including a total of 156 new inspectors. This means the Inspections Branch should be much better resourced in future to address emergencies, respond to complainants, and undertake its day-to-day inspection work within its established timelines. Expanding the number of inspectors is all the more important, given the government’s announcement that more than 31,000 new long-term care beds and 28,000 upgraded beds are in the process of being planned, constructed, and opened.
402 At the time the first wave of the pandemic hit, the Inspections Branch was significantly short-staffed. I am optimistic that the government’s commitment to increasing the staff resources available to the Inspections Branch will help ensure that the Branch is sufficiently resourced to fulfill its mandate in the years to come. To make certain this occurs, the Government of Ontario and the Ministry should work together to take all necessary steps to ensure sufficient inspectors and other personnel are hired and retained to carry out all necessary inspections within established timeframes. The Ministry should also carefully monitor and plan for staff vacancies to ensure they are quickly filled, so that the Branch maintains its resourcing in future.
Recommendation 44
The Government of Ontario and the Ministry of Long-Term Care should work together to ensure that, going forward, there are sufficient inspectors and other necessary staff to fulfill the Inspections Branch’s mandate within established timeframes.
Recommendation 45
The Ministry of Long-Term Care should carefully monitor and plan for staff vacancies to ensure they are quickly filled so that the Inspections Branch maintains its resourcing in the years to come.
Missing documentation
403 The Ministry ultimately carried out hundreds of inspections during the first COVID wave, using a mix of on-site, off-site, and “blended” approaches. According to the best available data, the Inspections Branch started 328 new inspections during the first wave and completed another 45-60 inspections it had paused at the start of the pandemic.
404 In many of these, the inspector’s job was made more difficult by a lack of care-related documentation for long-term care residents. Beginning on March 27, 2020, homes were allowed to stop documenting some care-related information. Specifically, the government introduced Ontario Regulation 95/20, which provided that:
Licensees are not required to document information unless it involves an incident of a significant nature or is required to ensure the proper care and safety of a resident.
Licensees are not required to immediately document changes to a resident’s plan of care…unless they involve changes of a significant nature or unless there are changes that staff members and others need to be aware of immediately.[117]
405 The government didn’t define the phrase “significant nature,” and the usual documentation requirements came back into force on July 15, 2020.[118] A press release announcing the new regulation and the name of the regulation itself (“Streamlining Requirements for Long-Term Care Homes”) explained that the purpose of these changes was to “help ensure there are enough staff to care for residents.”[119]
406 However, care-related documentation is an important source of information for inspectors, and its absence made it challenging for them to determine if a home was in compliance with the legislation, especially long after the fact. For instance, several inspectors told us how tough it was to inspect concerns about a resident’s nutrition, a common area of complaint. One said she found that personal support workers had gone days or even weeks without documenting residents’ intake. The lack of records, combined with the fact that the staff caring for individual residents frequently changed during this time, made it difficult to determine whether the home had complied with the legislation.
407 Other inspectors had similar stories, and it is clear the government’s decision to allow homes not to document information had a significant impact on inspections. As many pointed out, inspectors rely on point-in-time records and data to chart any changes in a resident’s condition and to determine if a home carried out the steps required under the law. Without this crucial information, they were often unable to confirm whether a home was in compliance. Given the importance of resident care information to Ministry inspectors, the Ministry and the Government of Ontario should ensure that documentation requirements related to resident care are not modified during any future emergency.
Recommendation 46
The Ministry of Long-Term Care and the Government of Ontario should ensure that documentation requirements related to resident care are not modified during any future emergency.
Inspecting infection prevention and control
408 In January 2022, a senior Inspections Branch manager told us during a briefing that from the onset of the pandemic, the Branch had included infection prevention and control (IPAC) as part of every inspection it conducted. This manager said inspectors spent 4-6 hours completing a checklist of IPAC-related items at every home, regardless of the type of inspection. We were told that if inspectors found any non-compliance related to IPAC, it would be included in the inspection report.
409 We also heard that Ministry inspectors worked closely with their public health counterparts to conduct co-ordinated IPAC assessments of many long-term care homes early in the first wave. These assessments were intended to identify potential issues and solutions, outside of the formal inspection process.
410 Our investigation revealed a different story. We found few examples – perhaps a dozen – where Ministry inspectors worked with public health officials to conduct IPAC assessments. Resourcing issues, a lack of PPE for inspectors, and reluctance by Ministry inspectors to participate in the assessments led to limited involvement in these joint efforts. And even when public health inspections occurred without Ministry involvement, there was no formalized way for sharing the results with the Ministry or incorporating that information into the Ministry’s own compliance activity. More recently, the Ministry has said it is exploring the idea of running pilot projects with public health units to try out formal models of co-ordination and collaboration – however, this has not happened yet.
411 Ombudsman investigators uncovered numerous examples where Ministry inspectors did not inspect IPAC issues while in a long-term care home for another reason. Although we did not look at every inspection report, we reviewed a random representative sample of 55 long-term care homes and considered the 2020 and 2021 inspection reports for those homes. We found that from May to December 2020, inspectors did not specifically inspect IPAC issues in the vast majority of cases. It was only in 2021 that they began routinely assessing IPAC adherence during their inspections.
412 When we put this information to the Ministry officials, they confirmed that the Inspections Branch only began assessing IPAC for all inspections on January 18, 2021, long after the first wave had ended. Since that date, Ministry inspectors have used a variety of checklists and guidance documents based on whether or not the home is in respiratory outbreak. Much of this guidance was developed by the Ministry’s long-term care consultant / environmental inspectors, who are long-term care inspectors and certified public health inspectors with special expertise in environmental or public health matters.
413 During the first wave, the Branch had three environmental inspectors who were able to assist with IPAC issues during an inspection. Unfortunately, according to an email we reviewed from a senior Branch manager, management forgot that these inspectors could assist with on-site inspections until June 3, 2020. On that day, the manager advised colleagues they could deploy two of the three for on-site inspections, and they occasionally did so shortly thereafter. For example, on June 5, Branch managers asked an environmental inspector to help the inspectors with IPAC issues at Woodbridge Vista Care Community. In another case the same month, an environmental inspector acted as secondary inspector during an inspection of the Pinecrest Nursing Home in Bobcaygeon that included a heavy focus on IPAC issues. Overall, though, requests for help from these specialized inspectors remained rare. Branch logs indicate that they were only asked to assist with IPAC-related issues on 10 occasions between November 2019 and November 2020.[120]
414 We heard contrasting views about what role inspectors should play in ensuring long-term care homes have adequate IPAC practices. Some felt public health units had greater expertise in this area and were better situated to do this work, while others believed there should be a co-ordinated approach involving the Inspections Branch, public health units, and inspectors from the Ministry of Labour, Immigration, Training and Skills Development.[121] Still others suggested that this work was clearly within the Ministry of Long-Term Care’s mandate of ensuring the safety of long-term care residents.
415 Despite its past practice of rarely using its environmental inspectors, the Ministry has recently acted to increase the IPAC expertise of the Branch by hiring additional environmental inspectors. We were told these positions will be distributed evenly across the province.
416 As the pandemic has made clear, robust infection prevention and control practices are essential for ensuring the health and safety of long-term care residents. The Ministry requires expertise among its inspections staff to adequately inspect infection prevention and control. The Branch should ensure that inspectors liaise when necessary with experts within the Branch, such as long-term care consultants / environmental inspectors, as well as those at local public health units. It should establish a policy setting out how and when inspectors should access these resources.
417 In addition, the Ministry should ensure that it co-ordinates with other organizations, such as public health units, to receive reports and assessments related to infection prevention and control in long-term care homes. The Ministry should clearly establish in policy how the information in these third-party reports will be used by Ministry inspectors.
Recommendation 47
The Ministry of Long-Term Care should ensure it has inspections staff with the necessary expertise to inspect infection prevention and control measures.
Recommendation 48
The Ministry of Long-Term Care’s Inspections Branch should ensure that inspectors liaise when necessary with infection prevention and control experts, both within the Branch and at public health units.
Recommendation 49
The Ministry of Long-Term Care should establish a policy setting out expectations for how and when inspectors will liaise with infection prevention and control experts, both within the Branch and at public health units, as well as the responsibilities of each organization.
Recommendation 50
The Ministry of Long-Term Care should ensure that it co-ordinates with other organizations, such as public health units, to receive reports and assessments related to infection prevention and control in long-term care homes.
Recommendation 51
The Ministry of Long-Term Care should clearly establish in policy how the information in third-party reports, including from public health units, will be used by Ministry inspectors.
Responding to Canadian Armed Forces concerns
418 On April 28, 2020, the Canadian Armed Forces (CAF) began to provide staffing support to five of the hardest-hit long-term care homes in the province: Altamont Care Community, Eatonville Care Centre, Holland Christian Homes Grace Manor (Brampton), Hawthorne Place Care Centre and Orchard Villa. On May 14, the CAF wrote to military leadership and federal government officials about serious and shocking conditions in these homes.[122] The observations reached the Ministry of Long-Term Care on May 24, 2020, and were shared with the Inspections Branch. When the CAF’s observations were made public a few days later, many senior government officials turned to the Inspections Branch for a plan to assess and respond to the serious observations.
419 The Branch immediately drafted a plan, setting out what concerns could be inspected for each home and how it would approach these inspections. Prior to the drafting of the plan, inspections were already in progress at four of the five CAF-supported homes. On May 27, the Ontario Government issued a news release, saying Ministry inspectors would go into the five homes to do “an expanded, stringent inspection process over a two-week period.”[123] Inspections of all five homes began by May 28, and according to the documents we reviewed, inspectors followed the usual Inspections Branch processes and inspection protocols when examining the issues raised by the CAF.
420 We heard that Ministry inspectors faced many challenges in examining the CAF’s concerns. The CAF observations did not generally include names and dates, and CAF personnel were initially reluctant to speak with inspectors. The Branch Director told us inspectors discovered that some CAF observations were based on opinion, rather than verifiable fact, and we were told the CAF later acknowledged this. The Branch Director also said that many of the CAF’s observations were serious issues that could be inspected.
421 In the end, the inspections at these homes took far longer than the promised two weeks, due to the number of issues examined at each home. The inspection reports were released between July 9 and August 26. Some of the Inspections Branch staff we spoke to indicated that many of the issues reported by the CAF were consistent with previous findings set out in Ministry inspection reports. They acknowledged the appalling content of the reports issued during the first COVID wave and the devastating scope of its consequences. However, they were confused about why the government and the public considered these to be new issues. One inspector commented:
Premier Ford said that the reports made by the CAF exposed shocking and horrific conditions for our seniors. We know that these things have been in our reports for years.
422 In a document we reviewed from early June 2020, a senior Branch manager shared similar feelings with colleagues:
Inspectors have been flagging similar concerns over the years. It’s all in inspection reports posted publicly. I think the issue is that CAF report was announced at a press conference by the Premier, so it got a lot more attention. Our inspection reports have always identified NC [non-compliance] issues with the homes.
423 Indeed, many of the homes supported by the CAF in the early days of the pandemic had previously been the subject of multiple inspections and repeated findings of non-compliance by Ministry inspectors, with no clear improvement on serious issues affecting resident care and safety. The CAF’s observations, and the Ministry’s subsequent inspections and findings, provide a chilling window into the conditions at some homes during the first wave, as well as the Ministry’s struggle to exercise its oversight role.
Altamont
424 One of the homes that the Ministry inspected in the wake of the CAF report was the 159-bed Altamont Care Community home in Scarborough. The CAF’s concerns included that residents were not receiving meals, some had wounds that were not cared for, and some were bed-bound for several weeks. The CAF also noted instances of unstable and inadequate staffing, staff failing to give residents their medications, nursing staff practicing unsafely, and much more.
425 The Inspections Branch treated the CAF observations as a “complaint” and categorized it at level 3+ in its triage risk system. Apparently, the Branch didn’t feel the issues warranted the highest risk level (4), despite the serious risk of harm to residents alleged in the report.
426 Ministry inspectors were on-site at Altamont between May 21 and June 30, 2020. On July 29, the Branch issued a 179-page inspection report, finding the home in non-compliance with 17 areas of the legislation.[124] Some of the key observations in the inspection report were:
- One personal support worker was responsible for caring for 97 residents in three wings of the home on a particular April day.
- Residents who were at risk of skin wounds were not being repositioned. One resident with a pressure ulcer[125] was “crying with pain” as a result. Another complained of “severe pain” after being left sitting up in a wheelchair for a prolonged period. Staff told inspectors that residents who couldn’t move on their own were generally left in bed when the home was short on staff.
- Unwell residents were placed in the same bedroom with those who were well, although there were empty bedrooms available within unoccupied areas of the home.
- Residents were left with “dirty hands, debris around the outside of eyes and mouths, dirty/stained clothing and/or wheelchairs and dirty feet,” after not being bathed or showered for a prolonged period of time. Later, after the home allowed residents to begin taking baths and showers again, an outside infection prevention and control (IPAC) team found the shower rooms were too unsanitary to use.
- The home generally did not document residents’ fluid intake levels on their plans of care because, according to the home’s dietitian, the “home’s corporate office, Sienna Senior Living, removed hydration status as a requirement within all residents’ plan of care a few years ago.”
- The home didn’t report the COVID outbreak to the Ministry as a “critical incident” for more than two months because its IPAC Lead erroneously thought such reports were not required due to the pandemic.
427 The inspection report also notes that things had likely been worse previously. During May and June 2020, the home had fewer residents than normal and more than its regular staffing complement, thanks to help from the CAF, the local hospital and an agency.
428 We also reviewed previously published Ministry inspection reports on Altamont, from before the pandemic. Although the pandemic magnified the scope of harm to residents, the home had been found in non-compliance on infection prevention and control, as well as skin and wound care during inspections in February 2019 and November 2019. According to those reports, inspectors found, among other things, staff not recording symptoms of resident infection on every shift, not wearing appropriate personal protective equipment (PPE), not washing hands, not reassessing residents at risk of skin breakdown, and not intervening immediately to help a resident with a skin wound.
429 On August 4, 2020 – just after the Branch published its inspection report on Altamont – the CAF provided an “exit report” to the Ministry. In it, the CAF said most of its initial concerns about Altamont had been resolved, or at least improved. However, it noted Altamont still had issues regarding the grouping (cohorting) of residents, incorrect charts, fluid intake for residents, and the availability of some supplies. We found no evidence that the Ministry issued any inspection reports for Altamont in relation to the CAF’s exit report.
Hawthorne Place
430 Of the five homes the CAF initially supported and reported on in May 2020, the 269-bed Hawthorne Place Care Centre in North York had the longest list of issues. The CAF’s concerns included numerous incidents of staff not using PPE properly, insect infestations, residents becoming soiled and experiencing skin breakdown because staff took too long to change them, “forceful and aggressive transfers,” “forceful feeding,” a feeding bottle left unchanged for so long that the contents turned “foul and coagulated,” staff not responding for more than two hours to residents who were crying for help, insufficient wound care supplies, and poor staff-to-resident ratios.
431 Ministry inspectors inspected Hawthorne Place between May 28 and June 24, 2020. The Branch issued its 91-page inspection report two months later, a delay a Ministry official attributed to the slow report writing speed of a newer inspector, and the need for collaboration and internal review.[126] In the report, the inspector found the home had not complied with six areas of the legislation:
- It did not ensure each resident had a plan of care that set out clear direction to staff about their needs, or that staff properly collaborated regarding those plans.
- It did not respond promptly to calls and alarms from residents.
- It did not ensure residents were turned and repositioned regularly or that they received immediate treatment for skin wounds. One staff member described being too busy serving snacks to reposition a resident.
- It did not ensure its staff participated in the infection prevention and control program. Inspectors saw staff incorrectly using personal protective equipment, including instances where they did not wear masks.
- It did not serve appropriate and safe food and drink items to some residents. On two occasions, inspectors watched staff serve residents drinks that the residents were allergic to.
432 As with Altamont, these issues at Hawthorne Place should not have been a surprise. Previous Ministry inspection reports had documented the home’s non-compliance with infection prevention and control requirements and skin and wound care.
433 There was one CAF observation that the Ministry did not originally inspect. The CAF specifically alleged that there had been resident deaths at Hawthorne Place due to dehydration and malnourishment. This information emerged only through the Long-Term Care COVID-19 Commission’s Final Report in late April 2021, nearly a year after the CAF’s first report.[127]
434 The Inspections Branch cannot investigate the cause of a resident’s death. However, Ministry inspectors sought information from the Office of the Chief Coroner and then inspected Hawthorne Place again, between May and July 2021. Inspectors reviewed the health records of residents who died during a specific time period, looking for evidence of non-compliance with the long-term care legislation. They found that staff at the home had not collaborated in their assessment of a specific resident who had returned from hospital, and who was not eating and drinking well. The Ministry inspectors issued a written notification to the home for that lapse, which is the least severe enforcement action and does not require any follow-up by inspectors.[128] The Ministry did not find any other non-compliance during its 2021 inspection.
Downsview
435 The CAF began supporting the 252-bed Downsview Long Term Care Centre home in North York later than other homes during the first wave. In this case, the Ministry inspected the home prior to the CAF’s support – from May 8-19, 2020. The resulting inspection report found the home in non-compliance with the legislation for failing to maintain a safe and secure home for residents.[129] The inspectors listed a series of lapses in the home’s infection prevention and control practices. They issued a compliance order, and also referred the matter to the Inspections Branch Director. They also issued compliance orders related to separate infection prevention and control issues and for end-of-life care. The week after the inspection, the Director issued a mandatory management order, requiring the home to retain the local hospital to manage it temporarily.
436 Almost a year later, it was revealed that the CAF had raised concerns about the care residents received prior to the CAF’s arrival. In 2021, the Long-Term Care COVID-19 Commission’s final report quoted CAF personnel saying “that 26 residents died due to dehydration prior to the arrival of the CAF team due to the lack of staff to care for them. They died when all they need[ed] was “water and a wipe down.”[130]
437 As with Hawthorne Place, the Inspections Branch asked the Office of the Chief Coroner for information regarding the residents who had died at Downsview and began its own inspection. Between May and July 2021, Ministry inspectors inspected the home again, looking for evidence of non-compliance with the long-term care legislation. The resulting inspection report found Downsview non-compliant in four areas: Not completing nutritional assessments for residents; not protecting residents from neglect; not looking after residents as required by their plans of care; and not complying with infection prevention and control measures. Inspectors issued compliance orders to the home on the first two items.[131]
438 Given the Branch’s mandate, the inspection report did not examine or comment on the residents’ cause of death. More recently, the CAF has backed away from the original suggestion that 26 of Downsview’s residents died of dehydration. In a written submission to our Office, the CAF said the allegation “was not based on direct observations made by members of the CAF but, rather, was based on concerns expressed during an informal discussion.” The CAF added that its team members did not conduct any investigations or autopsies into any resident deaths.
Failure to report
439 While the CAF’s concerns were eventually shared with the Inspections Branch, it is concerning that the Ministry did not inform CAF personnel that they were required by law to do so immediately.
440 At the time the CAF was supporting the homes, section 24 of the long-term care legislation required that any person[132] must “immediately” tell the Ministry of Long-Term Care Director if they have “reasonable grounds to suspect” certain conduct has taken place, including:
- Improper or incompetent treatment or care of a resident that resulted in harm or a risk of harm to the resident.
- Abuse of a resident by anyone or neglect of a resident by the licensee or staff that resulted in harm or a risk of harm to the resident.
- Unlawful conduct that resulted in harm or a risk of harm to a resident.[133]
441 Many of the CAF’s observations dated from April 28 to May 11, 2020, and involved neglect, improper treatment or care that led to residents experiencing harm or the risk of harm. The CAF documented and reported these concerns according to military orders and shared them with the relevant long-term care homes. However, the Ministry did not learn of them until May 24.
442 We asked the CAF if anyone in the government explained the requirement to make “mandatory reports” to the Ministry for the specific items listed in the legislation. We were told that CAF personnel received no specific training on reporting requirements under section 24 of the Long-Term Care Homes Act or the role of the Ministry’s Inspections Branch.
443 The Inspections Branch Director told us she was “shocked” by the CAF’s observations and described reaching out right away to inform them of the requirement to report to the Ministry. We also heard that the provincial emergency operations committee asked the CAF to ensure it reported concerns about long-term care homes directly to the Ministry and others “in a very timely manner”.
444 These requests seemed to have an effect. We saw numerous subsequent examples where the CAF reported concerns directly to the Ministry without delay. However, from April 28 to May 24, 2020 – when COVID was exacting a terrible toll on long-term care residents – the CAF was not promptly sharing its concerns with the Ministry. The Ministry should ensure that third-party organizations involved in managing or supporting long-term care homes know their legal obligation to report certain issues to the Ministry immediately. The Ministry should ensure these organizations are aware of the relevant legislative provisions, the items they must report, and how to make these reports.
Recommendation 52
The Ministry of Long-Term Care should ensure that all organizations involved in managing or supporting long-term care homes are advised of their legal obligation to immediately report certain issues to the Ministry.
Recommendation 53
The Ministry of Long-Term Care should ensure that all organizations involved in managing or supporting long-term care homes are aware of the items they must report to the Ministry and how to make these reports.
Enforcing Compliance
445 The Long-Term Care Homes Act, 2007 gave the Ministry’s Inspections Branch authority to impose a range of enforcement actions – or “penalties” – when inspectors found a home not complying with the law. Individual inspectors and the Inspections Branch Director had wide latitude in deciding what enforcement action to take in response to specific instances of non-compliance. Our investigation found that inspectors often chose to take a less serious enforcement action. We also found it was common for them to lower the default action that would otherwise apply, even for very serious contraventions of the law.
446 When the Branch did take action to require homes to fix non-compliance issues that were identified during the first wave, some inspectors gave homes many months to resolve serious issues that appeared to affect resident care and safety. The government has since made changes to enhance the severity and effectiveness of the Ministry’s enforcement options. However, it is important that the Branch operationalize these improvements carefully to ensure that they achieve the desired results.
Compliance basics
447 During the first wave of COVID, inspectors were required to take one or more specific enforcement actions when they found non-compliance with the Act.[134]
448 The Inspections Branch used a “Risk-Based Enforcement Model” to escalate enforcement when a long-term care home’s compliance with the law was poor. The model consisted of three pyramids, each with red, yellow and green bands.
449 If a home had high compliance with the law, the Ministry put fewer resources into enforcement. If a home had moderate compliance, the Ministry put more resources into enforcement, with the aim of “incenting and increasing compliance.” If compliance was low, the Ministry used a “high” level of resources for “effective, improved, meaningful enforcement.”
450 There were numerous enforcement actions the Ministry could take when non-compliance was found during this time, including:
- Written Notification: This is the minimum action taken by the inspector for every non-compliance. A written notification identifies the legislative reference and findings/reason the home was found non-compliant. The home is not required to take any specific action.
- Voluntary Plan of Correction: This requires the long-term care home licensee to prepare a written plan of correction for achieving compliance with the Act. There is no requirement for the licensee to submit the plan to the inspector or to produce the plan on subsequent inspections. As of April 2022, voluntary plans of correction are no longer an available enforcement mechanism.[135]
- Compliance Order: The Inspector or Branch Director may order a long-term care home licensee to do anything, or refrain from doing anything, to achieve compliance with a requirement under the Act. A licensee can also be required to prepare, submit and implement a plan for achieving compliance with a requirement under the Act. Long-term care homes can request that the Branch Director review a compliance order, and the Director can confirm, alter or rescind it. The Director’s decision can be further appealed to the Health Services Appeal Board.[136]
451 An inspector could also make a referral to a Director (“Director referral,” or sometimes “Director’s referral” in the Ministry’s parlance), which has no immediate consequence for the home, but may lead to the most serious enforcement actions. Inspectors must consult with management before taking this step. When a referral is made, the Director has the discretion to issue orders, including that a new manager be appointed to run the home, or that the home’s funding be stopped or its licence revoked.[137] Director’s orders may be appealed by long-term care homes to the Health Services Appeal and Review Board, which can rescind, confirm or alter them.[138]
452 Some offences under the long-term care legislation can be prosecuted under the Provincial Offences Act. For instance, failure to comply with certain orders is a provincial offence, regardless of the issue that originally prompted the Ministry to issue the order. Generally in such cases, individuals, directors and officers at long-term care homes face potential fines and/or imprisonment. Repeat offences can result in individual fines of up to $200,000, and corporations can face a $500,000 penalty.[139] We heard it is extremely rare for the Ministry to prosecute offences – no prosecutions were launched during the decade that the Long-Term Care Homes Act was in force. The Deputy Minister told us the Ministry did not have the practical capacity to mount a prosecution.
453 Since 2017, the long-term care legislation has also contained an enforcement tool known as administrative monetary penalties, which would allow the government to require homes to pay monetary penalties of up to $100,000 in response to findings of non-compliance.[140] However, these provisions of the legislation were not proclaimed in force before the pandemic. This enforcement tool is now available to the Ministry under the Fixing Long-Term Care Act, 2021.[141]
454 There are differing timeframes associated with each of the Ministry’s enforcement actions. Written notifications have none, because the Ministry does not follow up on those issues. If a home is ordered to create a plan for getting back into compliance, it is usually required to send that plan to the Ministry within 10 business days. The Ministry also gives the home a “compliance due date” – a deadline to complete the required items in the compliance order. During our investigation, these deadlines were 7, 21, 90 or 120 business days, depending on the priority of the issue and discussions with the homes. The Branch schedules a follow-up inspection – 30 or 60 business days after the due date – to make sure the home has made the required changes.
455 However, sometimes compliance cannot wait, and in specific situations, an inspector can issue an immediate order. At the start of the pandemic, inspectors were required to do this in “any circumstance where significant actual harm/risk, serious harm, or immediate jeopardy (risk)” was identified. The home was then required to fix the issue within a day, or before the inspector left the home.
456 We reviewed substantial data about the types of enforcement actions the Branch took to address non-compliance before the pandemic. The accompanying chart shows its actions in 2019 (arranged from least severe at the top to most severe at the bottom).
Number of Ministry of Long-Term Care enforcement actions taken in 2019
457 According to the Branch’s Inspections Reports policy, nearly every non-compliance results in a written notification (potentially in addition to other actions), so it is unsurprising to see so many issued. More than half of the findings of non-compliance also resulted in a voluntary plan of correction, which does not result in any follow-up from the Ministry. During 2019, fewer than 20% of the findings of non-compliance resulted in a compliance order, Director referral and/or a Director’s order, all of which require follow-up. That means for the other 80% of the cases where non-compliance was identified, the Ministry did not monitor further and had no knowledge of whether or not the homes addressed the issues.
“Judgement Matrix”
458 To determine which enforcement action to take in response to specific non-compliance during the first COVID wave, Ministry inspectors relied on a “judgement matrix” (attached at Appendix B). The Ministry has since moved to a different model for such decisions, although many of the relevant criteria remain the same.
459 To use the matrix, the inspector was first required to assign two scores for each non-compliance finding:
- Severity: The risk of harm the issue posed to residents. This ranged from 1 (least severe) to 4 (most severe). The definitions for each number are essentially the same as the triage risk levels, although level 3+ was absent.
- Scope: How pervasive the issue was in the home, from 1 (“isolated”) to 3 (“widespread”).
460 The inspector could alter/increase the severity score based on whether or not the issue was on a list of “key risk indicators” (items that posed a heightened risk of harm to long-term care residents), such as infection prevention and control.
461 The matrix then provided a range of possible enforcement actions according to the severity and scores, with one identified as the default. Inspectors had discretion to deviate from the default enforcement action based on the home’s compliance record for the previous 36 months – for instance, they could choose a more serious action in light of repeated non-compliance.
462 Inspectors were required to document their decision-making on a template document called the Judgement Matrix / Compliance Due Date Decision Tool. If the inspector issued a compliance order, they were also required to document how they determined the compliance due date. They were given wide latitude in determining what enforcement action to take in response to each instance of non-compliance.
Director referrals
463 The most serious enforcement action an individual inspector can take is to refer an issue to the Ministry’s Inspections Branch Director. During the first wave of the pandemic, inspectors issued 12 such referrals. Early in the pandemic, Ministry policy said a Director referral was “automatic” when:
- There is serious risk to resident(s); i.e., the inspector is issuing multiple “high risk” orders;
- A compliance order is being issued to the same home for the same non-compliance for the third consecutive time; or
- The appropriate response to a finding of non-compliance is beyond the authority of the inspector.
464 The policy on Director referrals changed as the pandemic progressed. As of February 2022, no situation requires an “automatic” referral. The revised policy directs the inspector and manager to consider four factors, including the enforcement action suggested by the Judgement Matrix, whether there has been repeated non-compliance, whether the situation is high risk, and whether the appropriate response to the non-compliance is beyond the authority of the inspector.
465 Inspectors must consult with management before making a referral to the Director. Once they decide to proceed, the inspector issues an order to the home and completes a form outlining the issues for Branch managers, as well as a package of supporting information. The inspector and managers meet with the Branch Director, who is ultimately responsible for deciding whether to proceed with any action. If the Director determines that action is not needed, the referral file is closed. There is no timeframe in which the Director must decide how to proceed, nor a requirement that the Director document reasons for such decisions.
466 The Director has several options for actions. These include asking the home for a compliance plan for fixing the issue (which the Ministry must receive and publish on its website), and/or making various orders, up to revoking the home’s licence. The Director can also hold a meeting with the long-term care home’s operator to go over the issues and explain what the home must do to achieve compliance.
467 Before the pandemic, issues of non-compliance with infection prevention and control requirements were rarely brought to the attention of the Inspections Branch Director. In 2019, there was only one such referral: The Village at St. Clair home in Windsor failed to monitor residents for infection on every shift and had not complied with two earlier Ministry compliance orders on the same issue.[142] After receiving this referral, the Director did not issue an order. Instead, the home submitted a compliance plan and held a meeting with Ministry officials, a follow-up inspection found it in compliance, and the matter was closed.
468 In 2020, there was just one Director referral for infection prevention and control issues. It was made just before the pandemic began and, remarkably, remained an open file through the first COVID wave. It related to a serious respiratory disease outbreak at Midland Gardens Care Community home in Scarborough, and came on the heels of previous inspections.
Midland Gardens
469 In 2019, there was a serious outbreak of respiratory disease in Midland Gardens Care Community, a long-term care home with 299 beds that is operated by Sienna Senior Living Inc. Three complaints about infection prevention and control were made to the Ministry’s Inspections Branch, prompting an inspection.
470 According to the Ministry’s inspection report about this outbreak, the home took several days to report to the Ministry and the local public health unit that residents and staff were experiencing symptoms of respiratory illness.[143] The inspection report explained that, had the home made its report earlier, the public health unit would have declared a respiratory outbreak and could have implemented measures “potentially limiting the additional spread of infection and enabling the outbreak to be under control sooner.” One resident died during the outbreak. The inspector concluded that the home had violated the law because it failed to ensure its staff participated in the infection prevention and control program.
471 The inspector issued a written notification and a compliance order to the home for this finding, and referred the issue to the Inspections Branch Director for further action. The inspector prepared an internal document to explain this referral, indicating that the home “failed to report outbreak symptoms” to the public health unit. They said staff were “unable to identify when and how to implement appropriate outbreak surveillance measures” and the inspection had found “no evidence” the home had done the staff training and education that the public health unit had previously recommended. They also noted that a similar finding against the home in 2017 had resulted in a voluntary plan of correction. The inspector found that a rapid turnover of leadership at the home had made it difficult to fix its problems, and that these issues posed a “serious and widespread risk” to residents.
472 The inspector recommended a “cease of admissions” at the home until the Branch could confirm its compliance with the latest order. This would have prevented the home from accepting new residents. A further document prepared by the Branch reiterated that the home was at a “high compliance risk level,” and suggested a mandatory management order in addition to prohibiting admission of new residents.
473 Ministry officials met in February 2020 to discuss these serious concerns. However, despite hearing that the home’s leadership was a “mess,” “not responsive,” and part of a “toxic culture” (according to notes from the meeting), the Inspections Branch Director did not issue any orders, nor stop admissions to the home. Instead, the Director opted to hold regular “status meetings” with the home.
474 On March 11, 2020, the Director and other Branch officials met formally with the manager of Midland Gardens. They confirmed to the home’s manager that instead of issuing a mandatory management order and preventing new admissions, they would hold regular status meetings with the home as a “piloting exercise.” According to the Branch’s meeting notes, those meetings would not be considered a follow-up inspection. Instead, the Branch saw the situation as an “opportunity to work in partnership and collaboration” with the home, with the aim of helping it achieve compliance.
475 The timing for this pilot exercise could not have been worse. Within days, COVID became the Branch’s focus and its attention shifted to supporting and monitoring long-term care homes throughout the province. The Director referral file for Midland Gardens stayed open, but apparently no action was taken on it between March and June 2020. During that period, Midland Gardens was overrun by respiratory disease caused by COVID-19. The home’s outbreak began on April 6, 2020. By June 14, the home had experienced more than 100 COVID cases – and 42 residents had died from the virus.
476 After inspections resumed, Ministry inspectors found more infection prevention and control issues at the home. In late June 2020, they found staff not wearing masks, wearing masks under their noses, and not wearing eye protection or using a barrier while screening visitors. They also saw staff move between residents without washing their hands. However, even these findings in the face of the ongoing pandemic did not prompt the Branch to take strong enforcement action. Instead, the inspector issued a written notification, which is the least severe enforcement action an inspector can take. The Director referral file on the same issue remained open; we do not know whether or not the Branch took account of this when deciding on her course of action.
477 In late July 2020, the Branch Director sent a letter to Midland Gardens about this open referral file, confirming that the next step would be regular “status meetings” with the home to support its plans to achieve and sustain compliance, as had been discussed at the March meeting. We were not able to confirm whether or when these meetings began. However, the Branch sent another letter in November 2020, indicating that follow-up inspections from September and October had found the home in compliance and that the Director referral would be closed.
478 Still, the home’s infection control troubles continued. Inspectors returned in April and May 2021, and – for the fourth time since 2017 – again found the home in contravention of infection prevention and control requirements. Despite this repeated violation of these regulatory provisions, the result of the inspection was a voluntary plan of correction, meaning there was no requirement for the Branch to go back to ensure the home corrected the issue.
479 We asked several Ministry officials about this case in an effort to better understand the Inspections Branch’s rationale for not using stronger enforcement tools at Midland Gardens. Unfortunately, those discussions did little to assist our understanding.
480 We also were unable to clarify whether the open Director referral impacted the Branch’s assessment of the risk within the home early in the pandemic. The records we reviewed indicate that even after the home’s COVID outbreak began, the Ministry assessed it at the lowest level of risk in its tracker. There was no mention of the IPAC-related referral to the Director, or the previous compliance orders about the same issue.
481 In Fall 2021, the Ministry updated its process for assessing COVID risk in long-term care homes to specifically take into account outstanding Director referrals or compliance orders related to infection protection and control. Had such a policy been in place in early 2020, the open referral for Midland Gardens might well have prompted the Ministry to do more, and sooner, and perhaps the home’s response to the first wave of the COVID-19 pandemic might have been more effective.
Altamont enforcement
482 Another case in which we questioned the potential role of a Director referral is that of the Altamont Care Community home in Scarborough, which was supported by the CAF, and where 53 residents died in the first COVID wave. When the Ministry conducted an inspection in the wake of the CAF’s spring 2020 report, it found 17 areas of non-compliance with the legislation, and made 26 distinct findings.[144]
483 For 20 of these 26 findings, Ministry inspectors lowered the “default” enforcement action set out in the Judgement Matrix. Many related to matters that were considered key risk indicators.
484 According to the Ministry’s records, for 12 of the 26 findings, the recommended default enforcement action was a Director referral. However, the inspectors decided to take a less serious enforcement action for all 12. In most cases, the justification for this variance was that no previous compliance order had been issued for the same matter. For one issue where a previous compliance order had been issued, the only reason provided for not making a Director referral was “will discuss with [inspections manager]”. There is no record of whether this discussion occurred and what it entailed. The manager in question had no recollection of any such discussion when we asked about it during our interviews.
485 It is hard to understand why the inspectors chose not to proceed with Director referrals in some instances. For instance, the inspection report included many pages of details about the home’s lax IPAC practices. Inspectors described staff not washing their hands or physically distancing and not wearing personal protective equipment (PPE) properly, a lack of PPE, and healthy and COVID-positive residents being kept together. It said these IPAC issues were widespread in the home. This was also the third time that Altamont had been found in non-compliance with IPAC requirements in a two-year period. The scores the inspectors assigned for these issues led to a default action of a Director referral. The report also documented other problems in the home, including a lack of cooling areas for residents.
486 Despite the seriousness of the scores and the home’s history of IPAC non-compliance, the Ministry inspectors ignored the default action of Director referral and issued “compliance order” instead – a choice that ruled out the more serious actions available to remedy the issues, such as through a Director’s order. Their stated reason was that the Branch had not previously issued a compliance order to the home for this issue.
487 On top of the 12 findings where the default “Director’s referral” (as it is called in the Judgement Matrix) was lowered to something else, there were eight other enforcement actions the inspectors also lowered. In all of those cases, the default action was a compliance order, but the inspectors lowered this to a voluntary plan of correction – which required no follow-up inspection to confirm the home had addressed the issue.
488 The inspectors also had the option to go beyond the default action for some of their findings in at least two cases, based on the home’s compliance history – but they chose not to do so.
489 For 11 of the 12 compliance orders they issued, the Ministry inspectors gave Altamont two months to fix the problems. For the 12th order – about a lack of cooling areas – they gave the home about three weeks. The reasons justifying these timeframes were not recorded. The “decision tool” document used by the inspectors should show the rationale for the chosen deadlines, but we discovered it was blank in every case.
490 When we asked Ministry officials for further information about the decision-making related to this inspection, their answers varied. One noted that by the time of the inspection, there was a voluntary management contract in place, which meant the home was under new day-to-day management. They also said that they trusted the judgment of the inspectors, who were very experienced. None of these explanations was documented in the Ministry’s records.
491 In the end, Altamont received:
- 17 written notifications – one for each area of the legislation the home was not in compliance with;
- 9 voluntary plans of correction; and
- 12 compliance orders.
492 In November 2020, the Ministry followed up on some non-compliance findings from the July 2020 inspection report, including the IPAC issues. Inspectors found that the home was in compliance on the issues identified, but also discovered new instances where it was non-compliant on other IPAC requirements.[145] Despite this being the fourth time Altamont was found non-compliant on IPAC issues in under two years, inspectors issued another voluntary plan of correction, requiring no follow-up inspection.
493 When we spoke with Ministry staff about this decision, they could not initially explain why the Branch did not escalate its enforcement action in light of the home’s repeated non-compliance. However, when we noted that the fourth inspection in November 2020 identified contravention of slightly different subsections of the same legislative sections regarding IPAC, we were told this was the rationale. The Ministry only considers it to be repeated non-compliance if it involves the exact same subsection. One official said: “Otherwise, some homes would never get out from [under] their orders.”
Pinecrest enforcement
494 The Ministry showed a similar lack of urgency at another home where inspectors found serious IPAC problems during the first COVID wave.
495 Pinecrest Nursing Home in Bobcaygeon is a relatively small long-term care home, with about 65 beds. It was the first long-term care home in Ontario to experience a large COVID outbreak. By the time it was declared over, 28 of the home’s 65 residents (more than 40%) had died.
496 The Ministry began its inspection of Pinecrest on June 8, 2020, after the outbreak ended. Its June 30 inspection report described a litany of IPAC-related problems, including:
- Staff and residents sitting close together and not wearing masks;
- Staff not changing their gloves as they moved throughout the home;
- Staff not putting on and taking off personal protective equipment properly; and
- A recently hospitalized resident returning from the hospital on contact/droplet precautions being placed in a room with another resident, even though there were empty rooms available.[146]
497 The inspection found the home’s IPAC practices in non-compliance and the report concluded:
The severity was a level 4 as immediate harm [to residents] was identified. The scope was a level 3, widespread, as the infection prevention and control program affects all residents and staff. The compliance history was a level 3, as the home had non-compliance under the same subsection.
498 For such high severity and scope scores, the Judgement Matrix recommended that the Ministry revoke the home’s licence and consider installing an interim manager while the home shuts down. According to Ministry policy, because the home had a recent history of non-compliance on IPAC, inspectors had no option to choose a less serious action.
499 Despite these findings and the requirements of the matrix, the Director did not revoke Pinecrest’s licence. In fact, the Branch did not even refer the case to the Director. Instead, the inspectors issued a compliance order requiring the home to:
- Revise its IPAC policies to ensure they reflect best practices;
- Retrain all staff on subjects such as hand hygiene, PPE, screening, surveillance, physical distancing, and self-isolation; and keep records of who has completed the training; and
- Develop a process to ensure all staff comply with the IPAC program.
500 Despite the conclusion that the issues presented “immediate harm,” inspectors gave the home until September 30, 2020 – three months – to complete the three items in the compliance order.
Lots of discretion, little urgency
501 Our Office saw numerous other examples where the Ministry took minimal action in response to serious non-compliance during the first wave of the pandemic, and set very long timeframes for homes to come back into compliance. An August 2020 inspection report made 11 findings of non-compliance at Hawthorne Place Care Centre, which had received support from the Canadian Armed Forces.[147] For two of these findings, the inspector took a less severe enforcement action than recommended by the Judgement Matrix. Ministry staff told us this was due, in part, to the Branch focusing on support and monitoring calls and the Ministry's inability to conduct a follow-up inspection, as well as consultation with Branch management. The home was given seven weeks to bring certain matters into compliance.
502 Ministry inspectors have the authority to issue “immediate orders” in certain circumstances that require long-term care homes to take urgent steps to resolve concerns. These types of orders are extremely rare. We found only two examples where they were used between March and December 2020. Current Ministry policy does not require inspectors to issue “immediate orders,” regardless of the conditions they find in a home. Inspectors have broad discretion when determining compliance due dates.
503 While some discretion is good and homes must be given a reasonable opportunity to fix problems, setting long compliance due dates means that residents must potentially live in substandard conditions for weeks or even months. To help address this issue, the Ministry should ensure that the Inspections Branch always issues an immediate compliance order for any situation where one or more residents are at an ongoing risk of serious harm. For cases that don’t pose immediate risk, the Branch should ensure that inspectors do not exceed the standard compliance due date timeframes, unless there is a clear and compelling reason to do so. This reason should be documented by the inspector, and the Ministry should require that any such extension be approved by a manager.
Recommendation 54
The Ministry of Long-Term Care should ensure that the Inspections Branch always issues an immediate compliance order for any situation where one or more residents are at an ongoing risk of serious harm.
Recommendation 55
For cases that don’t pose immediate risk, the Ministry of Long-Term Care’s Inspections Branch should ensure that inspectors do not set compliance due dates that exceed standard timeframes, unless there is a clear and compelling reason to do so.
Recommendation 56
The Ministry of Long-Term Care should require inspectors to document their clear and compelling reasons any time they set a compliance due date that exceeds the standard timeframe, and a manager should be required to approve this decision.
504 We also saw many examples where Ministry inspectors lowered the recommended enforcement action for a particular issue. While the policy also gave inspectors discretion to increase the action in certain instances, our investigation found that this was rare; most often, they reduced the enforcement action rather than raising it. Choosing a lower enforcement action had serious consequences, affecting what actions the home was required to take to resolve the issue, as well as its overall compliance record. The effects of taking less serious actions compound over time, as previous enforcement is a factor in determining subsequent enforcement actions.
505 According to a slide deck the Inspections Branch prepared for the Minister’s office, inspectors were supposed to “stay at median/default [recommended enforcement action] unless there is a strong rationale to adjust.” But our review of select Ministry inspection files suggests that inspectors routinely ignored the default action and substituted lower sanctions without any apparent justification.
506 It appears the government may have recognized this problem during the course of my Office’s investigation. The Ministry’s new policy, as of April 2022, no longer gives inspectors discretion to change the applicable enforcement action. This should assist in ensuring a robust, consistent approach to enforcement.
507 However, there is still substantial ambiguity about what types of issues should be dealt with through referrals to the Inspections Branch Director. As of early 2022, the Director Referral policy listed four criteria. Along with the guidance of the Judgement Matrix, these include whether there have been repeated contraventions after a compliance order, whether there is a high-risk situation, and whether the appropriate response to a finding of non-compliance is beyond the authority of the inspector.
508 Several of these criteria are inherently subjective, and inspectors are given limited guidance about what types of situations are contemplated by the policy. Director Referrals are the most serious action an inspector can take, and it is important that inspectors understand how to exercise this power. The Ministry should give managers and inspectors clearer guidance on when they should consider such a referral. The Branch should provide specific examples of different high-risk situations that should be brought to the Director’s attention, and guidance on situations that warrant action beyond an inspector’s authority.
Recommendation 57
The Ministry of Long-Term Care should modify the Director Referral policy to provide clearer guidance around when inspectors should consider making a referral.
Recommendation 58
The Ministry of Long-Term Care’s revised Director Referral policy should define what a “high-risk situation” means, and provide specific examples.
Recommendation 59
The Ministry of Long-Term Care’s revised Director Referral policy should provide clear direction regarding situations warranting an action beyond an inspector’s authority.
509 The Director Referral policy does not set out any timelines for the various steps in the referral process, nor require the Director to provide reasons for the decisions made. In the case of Midland Gardens, almost a year passed between the start of the inspection that prompted the referral to the Director and the closing of the file. Further, there was no explanation for why the Director ultimately decided not to proceed with any additional enforcement action despite significant infection prevention and control contraventions.
510 Any non-compliance that is subject to a Director referral is inherently serious in nature, and it is vital that the Branch promptly and fully address all referrals. The Ministry’s Inspections Branch should establish clear timeframes for this process and codify them in policy. The timeframes should be chosen to ensure that the Branch deals with these serious files as quickly as possible to mitigate the risk of harm to residents. In addition, the Ministry should ensure that the Inspections Branch Director documents all decisions made regarding enforcement action, and reasons to support them. In the interest of greater transparency, the Ministry should publish these reasons on the Ministry’s website. This would assist the public in understanding what steps have been taken in response to a finding of non-compliance and the supporting rationale.
Recommendation 60
The Ministry of Long-Term Care should develop a policy establishing clear timeframes for the Director Referral process, to ensure that serious files are addressed as quickly as possible to mitigate the risk of harm to residents.
Recommendation 61
The Ministry of Long-Term Care should ensure that the Inspections Branch Director records the reasons for their decision-making for every file that is referred to them.
Recommendation 62
In the interest of greater transparency, the Ministry of Long-Term Care should publish Director Referral decisions and relevant reasons on the Ministry’s website.
A new era of enforcement
511 When the Fixing Long-Term Care Act, 2021 came into force in April 2022, substantial changes were made to how the Ministry enforces compliance with the Act. The Inspections Branch also introduced a new policy and decision-making process for determining enforcement actions. Under the new policy, inspectors must assess three factors for every instance of non-compliance: Severity, scope and compliance history.
512 Based on these factors, inspectors use a “non-compliance decision” tool built into a template document (attached at Appendix C) to determine what enforcement action to take.
513 Under the new decision-making policy, voluntary plans of correction are no longer an available enforcement action as the new Act has removed this as an enforcement action. The Director referral option and the various Director’s orders are also absent. Instead, the policy now requires inspectors to consider the option of a Director referral whenever a written notification or compliance order is issued. If the inspector thinks a referral to the Director is warranted, they must discuss it with a manager. If the referral is made, the Director has discretion on what to do next, including potentially issuing one or more Director’s orders. However, inspectors no longer have discretion to vary the chosen enforcement action at the end of the process.
514 The design of the non-compliance decision-making tool means that the severity level will determine the appropriate enforcement action in the vast majority of cases, regardless of other factors. Given the importance of this determination, the Inspections Branch should ensure that inspectors receive robust training on how to assess the severity of harm that different forms of non-compliance cause to long-term care residents. In determining the “severity” of a particular issue, inspectors should focus on the health and well-being of residents and take into account the harm or risk of harm that an issue poses to them.
Recommendation 63
The Ministry of Long-Term Care should ensure that inspectors receive robust training on how to assess the severity of harm to long-term care residents caused by different forms of non-compliance.
Recommendation 64
In determining the “severity” of a particular issue, the Ministry of Long-Term Care should ensure that its policies and procedures require inspectors to focus on the health and well-being of long-term care residents and take into account the harm or risk of harm that an issue poses to those residents.
515 The new method for assessing non-compliance history offers the options “existing” or “none.” Determining whether there is “existing” non-compliance is very technical and depends on how the Ministry has classified a home’s non-compliance during the previous 36 months. The long-term care legislation is extremely detailed, with numerous sections, subsections, and paragraphs covering very similar matters. If a home has previously violated, for example, section 6(10)(b) of the legislation relating to plans of care, but on a subsequent inspection is found to have violated sections 6(10)(a) and 6(10)(c), the previous contravention would not be defined as “existing” non-compliance, even though all of these sections of the legislation address plans of care.
516 For sections of the legislation with dozens of subsections and paragraphs, this could potentially lead to absurd results. Rather than focusing on the specific legislative provision, the Ministry should amend its policy to ensure that inspectors look at any previous non-compliance at a home that relates to the same general subject matter as the issue they are examining. At a minimum, any previous non-compliance under the same section of the legislation within the last 36 months should count as previous non-compliance.
Recommendation 65
The Ministry of Long-Term Care should amend its policy to ensure that inspectors consider any previous non-compliance by a home that relates to the subject matter of the issue it is examining. At a minimum, any previous non-compliance under the same section of legislation within the last 36 months should count as previous non-compliance.
New enforcement tools
517 In addition to the revised decision-making tool, the Fixing Long-Term Care Act, 2021 also introduced new enforcement tools, as well as changes to existing enforcement options. Under the Act, a Ministry inspector or the Inspections Branch Director “may” impose an administrative monetary penalty on a home for not complying with the law. The Act and the new regulation together set out the details, including maximum fine amounts. Generally speaking, the more a home fails to comply with inspection findings, the more it may have to pay in penalties.[148]
518 Branch officials generally have discretion over whether to issue a monetary penalty, but they are required to do so when:
- The Ministry issues a compliance order for one of a specific list of items, and a follow-up inspection finds the home failed to comply with that order; and
- The Ministry finds a home non-compliant on an issue on which it had issued a compliance order in the previous three years.[149]
519 The Branch’s new enforcement policy provides inspectors with further guidance in issuing monetary penalties in these circumstances.
520 The Fixing Long-Term Care Act, 2021 also imposes higher penalties for homes that are successfully prosecuted, although the framework for undertaking prosecutions remains the same.[150] In May 2022, the Ministry told us it is building an “investigations unit” that will have a mandate to conduct investigations relating to the offence provisions in the new Act. This new function is intended to help the government address serious and repeated non-compliance by long-term care operators.
521 I am encouraged to see that the Government and the Ministry have taken steps to increase the availability of serious enforcement actions and penalties. Many government officials and long-term care stakeholders expressed concern to us that the Ministry’s previous approach did little to deter or punish poorly run homes. One senior official commented that even homes with a “horrible track record” faced “modest” consequences for their actions. The Auditor General and Long-term Care COVID-19 Commission both made similar observations and recommendations related to this issue.[151]
522 The Fixing Long-Term Care Act, 2021 also introduced three additional enforcement tools. The first allows the Branch Director and the Ministry of Long-Term Care to suspend a home’s licence, effective immediately.[152]
523 The second allows the Ministry to appoint a supervisor to manage a home. In some cases, this supervisor is akin to the “interim manager” that the Inspections Branch Director could install under the former legislation. However, under the Fixing Long-Term Care Act, 2021, the Lieutenant Governor in Council can also appoint the supervisor where the Minister decides to suspend a home’s licence. In that circumstance, the Lieutenant Governor in Council can specify the powers and duties of the supervisor. The Minister can also issue directions that the supervisor must carry out.[153]
524 The third new tool is a “re-inspection fee” of $500. The Regulation says the home must pay the fee whenever inspectors have to go back more than once to follow-up on a compliance order.[154]
525 At the same time, the new Act includes a way for inspectors to avoid taking enforcement action in response to findings of non-compliance. If a long-term care home corrects an area of non-compliance while Ministry inspectors are still at the home, the inspector can choose not to take any enforcement action if the issue caused no harm and created no risk or minimal risk of harm to a resident. The inspector must still document the non-compliance.[155]
526 Depending on how the Branch operationalizes this change, it could have cascading implications on future enforcement actions, which are often based on previous ones taken against a home. The Ministry should ensure that instances of non-compliance that do not result in enforcement action are considered when assessing future enforcement action against a long-term care home.
Recommendation 66
The Ministry of Long-Term Care should ensure that instances of non-compliance that do not result in enforcement action are considered when assessing future enforcement action against a long-term care home.
Inspection Reports
527 Inspection reports are the Ministry’s formal means of issuing enforcement actions to long-term care homes and documenting the results of an inspector’s work. When an inspector issues a compliance order to a home, the order is almost always included with the inspection report. Inspection reports are an important tool for helping homes, long-term care residents, their families and the public understand why the Ministry determined that a home was or was not in compliance with legislated requirements, and why a particular enforcement action was appropriate.
528 During our investigation, Ombudsman staff read hundreds of inspection reports. Although the Ministry says these reports should be accessible and use language that is as “clear as possible,” many were anything but.
529 Many reports we reviewed were lengthy, dense with acronyms, and poorly organized. Key information of interest was buried in different sections of the reports. Readers looking for all of the available information about a particular issue must search for it throughout the document – without the help of a table or contents or executive summary. Much of the information in these reports is automatically generated into a template from the Ministry’s internal software which it is in the process of overhauling.
530 There are many potential audiences for inspection reports, including long-term care homes, Ministry inspectors, residents and their loved ones. All would benefit from reports that are easier to navigate and understand. To assist in this goal, the Ministry’s Inspections Branch should add an executive summary at the start of each inspection report. The summary could outline the areas of non-compliance and the enforcement action(s) taken for each area. It could also explain to the reader which pages they should reference for more details on a specific area. If there are compliance orders associated with the inspection, the summary should also advise readers where to find them in the report.
Recommendation 67
The Ministry of Long-Term Care should add an executive summary to the start of its inspection reports that briefly outlines each area of non-compliance and the enforcement action(s) taken and includes relevant page references to help readers find more details about each specific issue.
531 Where possible, the Ministry should also ensure inspection reports are a reasonable length. The report on the Canadian Armed Forces’ complaint about the Altamont Care Community home was 179 pages, for example. Some extremely lengthy reports stem, in part, from the Ministry’s practice of reporting on several complaints and critical incidents at once, even if they are about different issues. For instance, the July 2020 inspection report about the Extendicare Guildwood home covered 10 different complaints. This not only adds to the length, but also makes it difficult for complainants to identify the findings related to their particular concerns. This potential confusion is compounded by the fact that the public reports are anonymized.
532 We were told that the Ministry recognizes some of these issues and has provided training to inspectors in August 2020 to assist in writing reports. The Ministry should continue to seek improvements to the clarity and readability of its inspection reports.
Recommendation 68
The Ministry of Long-Term Care’s Inspections Branch should ensure that inspection reports are as clear and concise as possible and written in such a way that individual complainants can easily determine how their specific concerns were reviewed by the Ministry.
533 At present, when a Ministry inspector finds no non-compliance related to a specific issue, very little information is provided in the report to support that finding or explain how it was reached. This can leave complainants – who are often the loved ones of residents – with no explanation of why their concerns were not substantiated. While it is important to document why a home has failed to comply with the legislation, there is also substantial value in explaining how the Ministry determined a home is in compliance. Making clear and supported findings that a home was following the law on a particular issue could also help instill public confidence in the home, as well as the Ministry’s oversight.
Recommendation 69
In cases where an inspection finds that a long-term care home is in compliance with the legislation, the Ministry of Long-Term Care should explain how it reached this determination.
534 It can also be difficult to determine whether or not compliance orders to a home have been resolved. The only practical way of doing this is to cross-reference the original inspection number and “compliance order number” and then search for those numbers in every subsequent inspection report published for that home. Some lucky readers will find a chart in a subsequent, unrelated inspection report showing that the home is back in compliance on that particular matter. However, no other details are provided. If an inspector found the home was still not in compliance, there is no simple way to track the outcome of the subsequent inspection.
535 Rather than report on compliance follow-up inspections as add-ons to unrelated inspection reports, the Ministry should report on them in separate, standalone inspection reports. These reports could include a brief outline of the original area of non-compliance, link back to the original report, and provide an explanation for why the home is (or is not) now in compliance. They could be specifically labelled as “follow-up inspections” on the Ministry’s website. Categorizing the reports in this way would make them easier for the public to find.
Recommendation 70
The Ministry of Long-Term Care should formalize follow-up inspections in standalone reports entitled “follow-up inspection reports,” which should include a clear description of the original issue that resulted in the compliance order, an explanation for why the home is or is not now in compliance, and whether other enforcement action is being taken.
Recommendation 71
The Ministry of Long-Term Care should post all follow-up inspection reports referred to in Recommendation 70 on its website.
536 It is sometimes necessary for the Ministry to amend inspection reports after they are issued. This commonly occurs when a long-term care home seeks a “Director’s review” of an inspector’s compliance order and the Director decides to rescind or alter the order. For example, the Director may decide to change the date by which the home must satisfy the order. When the Ministry amends an inspection report, it issues the amended report with a new date and with little to no explanation for why the amendment was made. It also removes the original report from its website. This can cause confusion, especially among members of the public, who often refer to inspection reports by the date they were first issued.
537 The Ministry should take steps to resolve this confusion and ensure that amended inspection reports are easily found and linked to their original version. It should also provide further explanation of what changed in the amended report and the reason for making the change, and ensure complainants are informed that a revised report has been issued.
Recommendation 72
The Ministry of Long-Term Care should ensure that when an inspection report is amended, it is clearly linked to the original version and that readers can easily find both inspection reports on the Ministry’s website.
Recommendation 73
The Ministry of Long-Term Care should provide further explanation for any amendment to an inspection report and clearly set out what has changed together with the reasons behind any changes.
Recommendation 74
The Ministry of Long-Term Care should inform complainants when an inspection report related to their complaint is amended.
Management Orders and Contracts
538 During the first few waves of the pandemic, the government asked hospitals to manage dozens of long-term care homes temporarily. These arrangements were most often formalized by mandatory management orders or voluntary management contracts. The former is a type of enforcement action and typically associated with specific contraventions found during an inspection of a home. A voluntary management contract is not an enforcement action but a private contract between a home and a temporary manager, with the Ministry’s approval.
539 Contrary to some media reports, these were not “government takeovers.” The Government of Ontario did not step in to run any of the homes itself. Rather, in facilitating these arrangements, the Ministry played an important role in supporting long-term care homes that were struggling with COVID-19. However, there were not always clear criteria for when a mandatory order should be put into place. During the first wave of the pandemic, as the government tried to respond quickly to the difficult conditions facing long-term care homes, the difference between voluntary contracts and mandatory orders became increasingly blurred.
Mandatory management orders
540 Mandatory management orders (MMOs) are a type of Director’s Order and are considered one of the most serious enforcement actions that can be imposed on a long-term care home. They require that a new manager be brought in to run the home. The Ministry must agree to the chosen manager, and the home owner (licensee) must pay for the manager’s services.[156]
541 At the start of the first COVID wave, the Long-Term Care Homes Act stated that the Ministry could issue a mandatory order when:
- The licensee failed to comply with a requirement under the Act; and
- There were reasonable grounds to believe that the licensee could not or would not properly manage the long-term care home or could not do so without assistance.[157]
542 At the start of the pandemic, the Ministry was not conducting inspections and could not find homes in non-compliance with the legislation. This meant the first requirement could not be met, and mandatory management orders were not an option. Homes that had rejected support even though they were clearly in crisis could not be forced to accept new management.
543 On May 12, 2020, however, the government introduced Ontario Regulation 210/20.[158] It gave the Inspections Branch Director broad authority to issue a mandatory management order (MMO) if there was a single laboratory-confirmed COVID case in a home.
544 With this change, the Ministry no longer needed evidence of non-compliance to issue an MMO. It used its expanded powers to issue three during the first wave:
- May 25, 2020: Downsview Long Term Care Centre in North York
- May 25, 2020: River Glen Haven Nursing Home in Sutton West
- June 2, 2020: Forest Heights in Kitchener
545 We were told that recommendations about which homes should be subject to MMOs were made at the province’s Incident Management System Table for Long-Term Care, with input from the ministries of Health and Long-Term Care, as well as Ontario Health. The table was established in April 2020 and met frequently during that time to guide the government’s response to pandemic-related issues in the long-term care sector. Since it had no authority to issue MMOs directly, it endorsed the recommendation and the Inspections Branch Director officially made the order.
546 These first-wave MMOs required local hospitals to manage the homes for 90 days, with the possibility of further extension. The homes had to submit a written management contract to the Ministry satisfying certain legal requirements, as well as a separate “recovery management plan.”
547 The Ministry told us these COVID-related MMOs would generally not count toward a home’s compliance history, as they could be issued without any specific findings of non-compliance confirmed through inspection.
Voluntary management contracts
548 On June 4, 2020, the Ministry began approving voluntary management contracts (VMCs) for some COVID-impacted homes.[159]
549 The concept of these voluntary contracts pre-dates the pandemic, and third-party managers have run many long-term care homes in Ontario for years. Prior to the pandemic, reasons for a VMC could vary. Some homes might prefer third-party management; others might be in need of management help.
550 The Ministry’s role in VMCs is usually limited. Staff from the Licensing Branch must review the contract to ensure it meets basic requirements and provide approval.
551 During the pandemic, there were no changes to this process, but the use of VMCs took on a different form. Unlike previous voluntary contracts, which were often for lengthy periods of time and not tied to a worldwide emergency, voluntary management contracts during the pandemic were for a short duration (e.g., 90 days), were arranged as a direct response to the impact of COVID, and the third-party manager was always a hospital. Hospitals do not typically have expertise in long-term care management, and the Ministry told us this was the first time it approved hospitals as temporary managers for long-term care homes. The contracts did not contain any information about why they were being put in place, or the conditions in the home at the time.
552 During the first wave, seven homes entered into VMCs with hospitals, with the approval of the Director of the Ministry’s Licensing Branch. Many others followed suit in the subsequent waves of the pandemic.
Truly voluntary?
553 Voluntary management contracts and mandatory management orders shared many characteristics during the first wave of COVID-19. They contained similar language and did not usually factor into a home’s compliance history. However, as a senior Ministry official told us, the homes generally viewed a VMC as preferable from a public relations perspective, and they potentially had more room to negotiate the terms, as opposed to an MMO.
554 The Ministry offered us various reasons why it issued mandatory management orders to some struggling homes, while allowing others to enter into voluntary contracts. We were told that VMCs were much faster to implement – some hospitals were able to start supporting homes even before the contracts were finalized. Others said a key factor was how the home responded to issues raised by the Inspections Branch. Senior officials on the Incident Management System Table for Long-Term Care told us some homes voluntarily agreed to a contract to avoid an MMO. We also heard that these decisions took into account whether a local medical officer had already issued the home with an order under the Health Protection and Promotion Act.
555 We were told that the Inspections Branch closely monitored each home under these COVID-related arrangements, and that Branch management had frequent meetings to discuss the issues at these homes and the progress being made. As the VMCs and MMOs reached their end points, the Inspections Branch was also responsible for assessing whether the homes could manage themselves. The Branch created a standardized process, documented on a “Transition and Sustainability Checklist,” that considered factors such as staffing, IPAC education and adherence, emergency plans, and clinical care. Based on these assessments, hospitals continued to officially manage several long-term care homes – and informally supported many more – well beyond the initial 90 days.
556 In June 2021, the Inspections Branch implemented a new policy (the “COVID-19 – Director’s Orders and Decisions Policy”) to formalize its involvement with COVID-related mandatory orders and voluntary contracts. A home must be in COVID outbreak for such an arrangement. The policy says decisions will be made on a “case-by-case basis” but should be consistently managed. It sets out separate processes and procedures for COVID-related VMCs and MMOs. In both cases, the temporary manager must submit a “recovery management plan” to the Inspections Branch Director within five days of being named. Fifteen days before the arrangement ends, the temporary manager must provide a transition plan for the Branch Director’s review and approval.
557 The Fixing Long-Term Care Act, 2021 gives the Ministry much greater discretion when issuing mandatory management orders. As before, the Ministry can issue an MMO whenever a home has not complied with a requirement under the Act. The new Act also allows the Ministry to issue one when a home is experiencing an emergency, including an outbreak of disease of public health significance, or when there are circumstances in the home that are “prejudicial” to the health, safety or welfare of residents. It also gives the Ministry the choice to order a new manager for the home as a whole or to seek a manager for a specific issue only.[160] These changes provide enhanced flexibility for issuing mandatory orders to long-term care homes.
558 What is lacking from this new framework is specific guidance on how the Ministry will exercise its powers in practice. To encourage consistency and predictability in decision-making, the Ministry should ensure there are specific criteria to guide the issuance of MMOs, including reference to how inspection-related information will factor into its decisions, the role of the Inspections Branch in monitoring the orders, and whether and how these orders will impact a home’s compliance history.
Recommendation 75
The Ministry of Long-Term Care should develop specific criteria to guide the issuance of mandatory management orders, including reference to how inspection-related information will factor into its decisions, the role of the Inspections Branch in monitoring the orders, and whether/how these orders will impact a home’s compliance history.
Opinion
559 The Ministry of Long-Term Care exists to ensure the safety and well-being of the nearly 80,000 residents who live in long-term care homes. These residents are some of the most vulnerable Ontarians and largely rely on others to meet their basic needs. Even before the pandemic, the system struggled to ensure that residents’ needs were met, with the Gillese Inquiry describing the long-term care sector as “strained but not broken.”[161]
560 COVID-19 upended this delicate balance, and in just a few short months almost 2,000 residents died from the virus. As this tragedy unfolded in real time, Ministry inspectors were almost nowhere to be seen. For at least seven weeks, and up to three months in one area, they did not conduct any on-site inspections, despite receiving an influx of complaints and questions about serious, potentially deadly issues. The Ministry was woefully unprepared to conduct inspections during a pandemic because it hadn’t planned for one. Inspectors did not have infection protection and control training, and the Ministry had no personal protective equipment supply to keep inspectors safe. Even once these issues were resolved, there was no plan for how inspectors would be deployed, and for lengthy periods the Ministry relied on a small number of volunteers to inspect a huge number of homes that had COVID outbreaks.
561 Our investigation identified problems with nearly all aspects of the Inspections Branch process during the first COVID wave. The Ministry was unprepared for a deluge of COVID-related complaints and questions and did not give inspectors practical guidance about how the pandemic should affect its triage and risk assessment process. Concerns surrounding PPE, staffing, and infection prevention and control were rarely considered high risk. Many people who tried to make complaints about the conditions faced by loved ones in long term care received “key messages” from inspectors and had their files closed without further review or inspection. The surge in complaints also exposed serious issues in the documentation and communication practices at the Branch, leaving it without vital information at a critical time. Complaints are crucial to guiding the work of the Inspections Branch, and the breakdown in the system for receiving, assessing and responding to them had a profound impact on the ability of the Branch to ensure the safety of long-term care staff and residents during the pandemic.
562 The Ministry also conducted no inspections into critical incidents involving COVID outbreaks until June 2020, and took limited enforcement action in response to homes that were not submitting critical incident reports as required. While it is impossible to know what difference a more robust process could have made, the Ministry clearly lost a valuable opportunity to inspect and intervene when homes reported outbreaks.
563 When the Ministry eventually conducted inspections and found violations of the law, it often took limited enforcement action. Our investigation found that the Inspections Branch often chose to take the least severe enforcement action available. Moreover, it was common for inspectors to lower the default enforcement action, even for extremely serious instances of non-compliance. When the Branch did take action to require homes to fix issues identified during first-wave inspections, inspectors gave homes many months to fix significant issues. These inspections and any resulting enforcement actions were documented in reports that were lengthy, dense with acronyms, and poorly organized.
564 Fundamentally, the purpose of inspection and enforcement is to keep long-term care home residents and staff safe. The Ministry’s goal should always be to confirm that homes are complying with legislated requirements, and if not, to bring them back into compliance as soon as possible while encouraging future compliance. Ensuring the safety of residents and staff must be the primary mission of the Branch and reflected in its work culture.
565 Although there are multiple organizations involved in overseeing long-term care homes, the Ministry of Long-Term Care has primary responsibility for ensuring that the care residents receive is consistent with the law. During the pandemic’s first wave, when the stakes were arguably the highest they have ever been, the Ministry was unprepared and unable to ensure the safety of long-term care residents and staff. It is my opinion that this was unreasonable, unjust, and wrong under sections 21(1)(b) and (d) of the Ombudsman Act.[162]
566 While this investigation was underway, the government made numerous changes that affect the work of the Inspections Branch. New legislation gives inspectors more tools to enforce compliance, and the government has substantially increased staffing within the Branch. I am hopeful that these changes will assist in addressing the issues identified in my investigation, and my Office will monitor the government’s commitment to these initiatives carefully as memories of the early days of the pandemic begin to fade.
567 I have also called on the Government of Ontario to take additional action to reinforce the long-term care sector and strengthen its ability in future to respond to crisis. Towards this goal, I have recommended revision to legislation to improve whistleblower protection and expand the circumstances in which homes must report critical incidents. I have encouraged the Government to work with the Ministry to ensure the Inspections Branch has sufficient inspection and other staff necessary to carry out its mandate. I have also recommended that in future emergencies, homes should not be relieved of the responsibility to properly document resident care.
568 COVID-19 will not be the last pandemic for Ontario’s long-term care homes. The Ministry of Long-Term Care must continue to implement significant improvements and commit to remembering the lessons from this experience in order to ensure the safety of residents and staff when the next threat emerges. Long-term care residents, staff, their loved ones, and all Ontarians deserve nothing less.
569 I will monitor the Ministry of Long-Term Care’s progress in implementing my recommendations.
Recommendation 76
The Ministry of Long-Term Care should report back to my Office in six months’ time on its progress in implementing my recommendations, and at six-month intervals thereafter until such time as I am satisfied that adequate steps have been taken to address them.
Recommendations
570 The next pandemic could come sooner than we think and be even deadlier than the COVID-19 pandemic. Effective preparedness and strong oversight are absolutely essential to mitigating risk.
571 I make these recommendations with the aim of building on the work that has been done to date and continuing to improve the Ministry of Long-Term Care’s oversight of long-term care homes, and thus the health and safety of residents and staff:
Recommendation 1
The Ministry of Long-Term Care should ensure that the Inspections Branch always has inspectors immediately available to inspect on-site at long-term care homes.
Recommendation 2
The Ministry of Long-Term Care should establish a policy clearly setting out what types of issues can be inspected using an off-site process, or a blended off-site and on-site approach. The policy should also identify circumstances were an on-site inspection is always required.
Recommendation 3
The Ministry of Long-Term Care should work with long-term care homes to ensure that the Inspections Branch can remotely access long-term care homes’ records electronically without delay.
Recommendation 4
The Ministry of Long-Term Care should work with long-term care homes to establish a procedure for remotely interviewing long-term care home staff or residents that considers the importance of privacy and video communication.
Recommendation 5
The Ministry of Long-Term Care should work with relevant government organizations to develop a policy on requirements for infectious disease testing for inspectors.
Recommendation 6
The Ministry of Long-Term Care should share the policy referred to in Recommendation 5 with the long-term care sector, the union representing inspectors, and other stakeholders.
Recommendation 7
The Ministry of Long-Term Care’s Inspections Branch should develop a policy covering movement between long-term care homes when inspectors have visited homes experiencing outbreaks of infectious disease.
Recommendation 8
The Ministry of Long-Term Care should amend its Preparing for On-Site Inspections During a Pandemic policy so it clearly defines when inspectors will work on- and off-site during pandemics and similar crisis situations, and what criteria will factor into that decision.
Recommendation 9
The Ministry of Long-Term Care should also amend this policy to establish who will be responsible for making criteria-based decisions about on-site versus off-site inspections during a pandemic and how these decisions will be communicated to long-term care homes and the public.
Recommendation 10
The Ministry of Long-Term Care should develop and implement a specific policy regarding the procurement, storage, and use of personal protective equipment (PPE). The Ministry should ensure that its approach will provide inspectors with adequate supplies of PPE to continue the Ministry’s operations even during periods of acute shortage.
Recommendation 11
The Ministry of Long-Term Care should also proactively engage with other provincial organizations responsible for managing strategic PPE supplies to ensure that the needs of Ministry Long-Term Care inspectors will be appropriately prioritized in the case of a future pandemic.
Recommendation 12
The Ministry of Long-Term Care should ensure a clear separation of responsibilities so that functions that don’t involve inspections/compliance work are not done by inspectors, to avoid confusion and conflict regarding the inspection function.
Recommendation 13
If the Ministry of Long-Term Care requires data from long-term care homes to monitor and respond to emergency conditions, it should co-ordinate with other organizations that may be collecting or have access to similar information, to ensure there is better communication and information sharing and no unnecessary duplication.
Recommendation 14
When faced with new or emerging threats in long-term care homes, such as a novel disease, the Ministry of Long-Term Care should provide inspectors and other staff with guidance and training on the risk that the threat poses to long-term care residents.
Recommendation 15
When new or emerging threats are active, the Ministry of Long-Term Care should adapt its triage risk levels to reflect the risk that the threat poses to long-term care residents.
Recommendation 16
The Ministry of Long-Term Care should provide staff with practical examples of what types of issues related to the new threat should be triaged at each risk level.
Recommendation 17
The Ministry of Long-Term Care should ensure inspectors are required to record specifically what level of risk a complaint was found to pose, prior to closing the complaint file in the Ministry’s documentation system.
Recommendation 18
The Ministry of Long-Term Care should amend the Inspections Branch’s policies and protocols to require inspectors to take a broad and inclusive approach to the complaint issues they can inspect, and to clearly state that the Branch has the authority to inspect any complaint that indicates a resident may be at risk of harm as a result of the home’s acts or omissions.
Recommendation 19
The Ministry of Long-Term Care should ensure that complaint files record the complete substance of all communications related to the file, including with the complainant, the long-term care home, and third parties.
Recommendation 20
The Ministry of Long-Term Care should examine options to audio record the Branch’s calls to complainants, and retain audio records in complaint files to ensure more accurate and complete records and assist management when auditing files for quality and training purposes.
Recommendation 21
The Ministry of Long-Term Care should ensure that any information relied on when deciding how to respond to a complaint is clearly documented in the complaint file.
Recommendation 22
The Ministry of Long-Term Care should conduct regular audits of files to ensure that it is consistently meeting its service standard of responding to all complaints within one business day.
Recommendation 23
The Ministry of Long-Term Care should introduce a policy specifying the situations in which Ministry inspectors should reach out to public health units regarding complaints and the information that may be shared with public health units in certain circumstances.
Recommendation 24
The Ministry of Long-Term Care should work with public health units to clarify the public health units’ role regarding long-term care home inspections during any future public health emergency.
Recommendation 25
The Ministry of Long-Term Care should proactively educate public health units about the role of the Inspections Branch, including providing examples of which complaints should be referred to the Branch.
Recommendation 26
The Ministry of Long-Term Care should remove “support” from the name of its complaints line and adopt a name that accurately reflects that the purpose of the line is to enable individuals to file complaints that the Ministry can review and act upon.
Recommendation 28
The Ministry of Long-Term Care should direct staff to document whether a file is a question, request for information or a complaint.
Recommendation 29
The Ministry of Long-Term Care should keep separate statistics for complaints and for requests for information.
Recommendation 30
The Ministry of Long-Term Care should ensure that the inquiry process is only relied on for issues that genuinely present little or no risk to long-term care residents. Issues that present greater risk should be inspected, as required by Ministry policy.
Recommendation 31
The Ministry of Long-Term Care should enhance its process for assessing trends to ensure that it takes into account situations where the same issue has been raised in connection with different residents of the same home.
Recommendation 32
The Ministry of Long-Term Care should also ensure that inspectors have flexibility to assess trends over longer periods in instances where the issue may arise seasonally.
Recommendation 33
The Ministry of Long-Term Care should take steps to ensure Branch managers are aware of and comply with the requirement to audit inquiry files.
Recommendation 34
The Ministry of Long-Term Care should increase management oversight for closing inquiry files. For instance, the Ministry could increase the percentage of inquiry files that managers must audit, or it may require a manager’s approval for closing an inquiry file.
Recommendation 35
The Ministry of Long-Term Care should direct inspectors to inform homes of any instances of non-compliance identified during inquiries and ensure they are appropriately documented and considered as part of the home’s compliance history.
Recommendation 36
The Ministry of Long-Term Care should ensure that long-term care residents can always meaningfully access complaint avenues during disease outbreaks and other emergencies.
Recommendation 37
The Government of Ontario should revise the whistleblowing protections in section 117 of O. Reg. 246/22 under the Fixing Long-Term Care Act, 2021, so that its protections clearly apply to concerns raised about a long-term care home to any applicable body, including the Ministry of Long-Term Care, public health units, the Patient Ombudsman, the Office of the Ontario Ombudsman, and the long-term care homes themselves.
Recommendation 38
The Ministry of Long-Term Care should develop a written process to better protect whistleblowers’ identity, including establishing procedures to protect whistleblower files, and it should publish information about these processes and the relevant legislation on its website.
Recommendation 39
The Ministry of Long-Term Care should amend its policy regarding cases of alleged retaliation to provide inspectors with greater flexibility regarding evidence that would support a finding of retaliation.
Recommendation 40
The Ministry of Long-Term Care should not take into account any prior self-assessments conducted by a long-term care home when deciding whether an immediate inspection is warranted in response to a COVID-related critical incident report.
Recommendation 41
The Government of Ontario should amend the regulations under the Fixing Long-Term Care Act, 2021 to include a category covering situations where residents are at risk of serious harm, whatever the cause, in the list of circumstances requiring long-term care homes to file critical incident reports with the Ministry of Long-Term Care.
Recommendation 42
The Ministry of Long-Term Care should consistently track when inspections begin, monitor whether it is meeting its inspection timelines, and take any necessary remedial action.
Recommendation 43
The Ministry of Long-Term Care should also provide staff with clarification on how to interpret the inspection timelines.
Recommendation 44
The Government of Ontario and the Ministry of Long-Term Care should work together to ensure that, going forward, there are sufficient inspectors and other necessary staff to fulfill the Inspections Branch’s mandate within established timeframes.
Recommendation 45
The Ministry of Long-Term Care should carefully monitor and plan for staff vacancies to ensure they are quickly filled so that the Inspections Branch maintains its resourcing in the years to come.
Recommendation 46
The Ministry of Long-Term Care and the Government of Ontario should ensure that documentation requirements related to resident care are not modified during any future emergency.
Recommendation 47
The Ministry of Long-Term Care should ensure it has inspections staff with the necessary expertise to inspect infection prevention and control measures.
Recommendation 48
The Ministry of Long-Term Care’s Inspections Branch should ensure that inspectors liaise when necessary with infection prevention and control experts, both within the Branch and at public health units.
Recommendation 49
The Ministry of Long-Term Care should establish a policy setting out expectations for how and when inspectors will liaise with infection prevention and control experts, both within the Branch and at public health units, as well as the responsibilities of each organization.
Recommendation 50
The Ministry of Long-Term Care should ensure that it co-ordinates with other organizations, such as public health units, to receive reports and assessments related to infection prevention and control in long-term care homes.
Recommendation 51
The Ministry of Long-Term Care should clearly establish in policy how the information in third-party reports, including from public health units, will be used by Ministry inspectors.
Recommendation 52
The Ministry of Long-Term Care should ensure that all organizations involved in managing or supporting long-term care homes are advised of their legal obligation to immediately report certain issues to the Ministry.
Recommendation 53
The Ministry of Long-Term Care should ensure that all organizations involved in managing or supporting long-term care homes are aware of the items they must report to the Ministry and how to make these reports.
Recommendation 54
The Ministry of Long-Term Care should ensure that the Inspections Branch always issues an immediate compliance order for any situation where one or more residents are at an ongoing risk of serious harm.
Recommendation 55
For cases that don’t pose immediate risk, the Ministry of Long-Term Care’s Inspections Branch should ensure that inspectors do not set compliance due dates that exceed standard timeframes, unless there is a clear and compelling reason to do so.
Recommendation 56
The Ministry of Long-Term Care should require inspectors to document their clear and compelling reasons any time they set a compliance due date that exceeds the standard timeframe, and a manager should be required to approve this decision.
Recommendation 57
The Ministry of Long-Term Care should modify the Director Referral policy to provide clearer guidance around when inspectors should consider making a referral.
Recommendation 58
The Ministry of Long-Term Care’s revised Director Referral policy should define what a “high-risk situation” means, and provide specific examples.
Recommendation 59
The Ministry of Long-Term Care’s revised Director Referral policy should provide clear direction regarding situations warranting an action beyond an inspector’s authority.
Recommendation 60
The Ministry of Long-Term Care should develop a policy establishing clear timeframes for the Director Referral process, to ensure that serious files are addressed as quickly as possible to mitigate the risk of harm to residents.
Recommendation 61
The Ministry of Long-Term Care should ensure that the Inspections Branch Director records the reasons for their decision-making for every file that is referred to them.
Recommendation 62
In the interest of greater transparency, the Ministry of Long-Term Care should publish Director Referral decisions and relevant reasons on the Ministry’s website.
Recommendation 63
The Ministry of Long-Term Care should ensure that inspectors receive robust training on how to assess the severity of harm to long-term care residents caused by different forms of non-compliance.
Recommendation 64
In determining the “severity” of a particular issue, the Ministry of Long-Term Care should ensure that its policies and procedures require inspectors to focus on the health and well-being of long-term care residents and take into account the harm or risk of harm that an issue poses to those residents.
Recommendation 65
The Ministry of Long-Term Care should amend its policy to ensure that inspectors consider any previous non-compliance by a home that relates to the subject matter of the issue it is examining. At a minimum, any previous non-compliance under the same section of legislation within the last 36 months should count as previous non-compliance.
Recommendation 66
The Ministry of Long-Term Care should ensure that instances of non-compliance that do not result in enforcement action are considered when assessing future enforcement action against a long-term care home.
Recommendation 67
The Ministry of Long-Term Care should add an executive summary to the start of its inspection reports that briefly outlines each area of non-compliance and the enforcement action(s) taken and includes relevant page references to help readers find more details about each specific issue.
Recommendation 68
The Ministry of Long-Term Care’s Inspections Branch should ensure that inspection reports are as clear and concise as possible and written in such a way that individual complainants can easily determine how their specific concerns were reviewed by the Ministry.
Recommendation 69
In cases where an inspection finds that a long-term care home is in compliance with the legislation, the Ministry of Long-Term Care should explain how it reached this determination.
Recommendation 70
The Ministry of Long-Term Care should formalize follow-up inspections in standalone reports entitled “follow-up inspection reports,” which should include a clear description of the original issue that resulted in the compliance order, an explanation for why the home is or is not now in compliance, and whether other enforcement action is being taken.
Recommendation 71
The Ministry of Long-Term Care should post all follow-up inspection reports referred to in Recommendation 70 on its website.
Recommendation 72
The Ministry of Long-Term Care should ensure that when an inspection report is amended, it is clearly linked to the original version and that readers can easily find both inspection reports on the Ministry’s website.
Recommendation 73
The Ministry of Long-Term Care should provide further explanation for any amendment to an inspection report and clearly set out what has changed together with the reasons behind any changes.
Recommendation 74
The Ministry of Long-Term Care should inform complainants when an inspection report related to their complaint is amended.
Recommendation 75
The Ministry of Long-Term Care should develop specific criteria to guide the issuance of mandatory management orders, including reference to how inspection-related information will factor into its decisions, the role of the Inspections Branch in monitoring the orders, and whether/how these orders will impact a home’s compliance history.
Recommendation 76
The Ministry of Long-Term Care should report back to my Office in six months’ time on its progress in implementing my recommendations, and at six-month intervals thereafter until such time as I am satisfied that adequate steps have been taken to address them.
Response
572 The Ministry of Long-Term Care and the Ministry of Health were given an opportunity to review and respond to a preliminary copy of my report, including my findings, opinion, and recommendations. The Canadian Armed Forces were also given an opportunity to review and respond to portions of the report related to their organization. All comments we received were taken into consideration in the preparation of this final report.
573 Writing on behalf of both Ministries, the Deputy Minister of Long-Term Care accepted all of my recommendations. The Deputy Minister said that more than half of the recommendations have already been fully or partially implemented, and that the Ministry is committed to evaluating the others to determine how they can best be realized. She explained that the Ministry has undertaken significant work in recent years, and that further improvements will be informed by this report’s recommendations. The Deputy Minister concluded by noting that the Ministry is committed to working in partnership with my Office, long-term care homes, and other ministries to help ensure that every long-term care resident experiences the best possible quality of life, supported by safe, high-quality care. A copy of the Ministry’s response is appended to this report.
574 I am pleased by the Ministry’s positive reply to my report and its commitment to improving its oversight of the long-term care sector. The Ministry has agreed to provide my Office with semi-annual status updates, and we will closely monitor its progress in implementing my recommendations.
________________________
Paul Dubé
Ombudsman of Ontario
Appendix A: Chronology of the Crisis
Timeline of key events affecting the work of the Ministry of Long-Term Care’s Inspections Branch during the first wave of the COVID-19 pandemic.
| Date | Key event |
|---|---|
| March 2020 | |
| March 9 | In light of growing concerns about COVID-19, the Ministry of Long-Term Care and its Inspections Branch updated their “Continuity of Operations Plan” documents. The updated versions didn’t provide direction on how to conduct inspections during a pandemic. |
| March 11 | The World Health Organization declared COVID-19 a pandemic. |
| March 13 | The Secretary of Cabinet directed the Ontario Public Service – including the Inspections Branch – to work from home for three weeks. Inspections immediately stopped. |
| March 16 | Ministry of Long-Term Care inspectors began working from home. They worked on finalizing their outstanding inspection reports and awaited further instructions. The Inspections Branch asked them not to make inquiries with homes and not to issue inspection reports. |
| March 17 | The Inspections Branch prepared a plan for the Deputy Minister’s office. It suggested continuing high-risk inspections only, largely off-site. Its list of high-risk scenarios included nothing specific to COVID. |
| March 18 | The Inspections Branch Director asked inspectors to begin making “support and monitoring” calls to long-term care homes to gather information. The Branch also asked inspectors to start contacting complainants directly and conduct intake of complaints. This job was previously performed by triage officers. The Director provided inspectors with “key messages” to help inspectors when speaking with complainants. |
| March 18 – 19 | The Inspections Branch put its “COVID-19 Emergency Inspection Policy” in place. It called for off-site inspections in all but the most extenuating circumstances. No off-site inspections were started. |
| March 21 | The Premier’s Office and Cabinet Office approved the Inspections Branch’s plan for inspections during the pandemic. The Deputy Minister believed some on-site inspections were continuing. |
| March 25 | The Inspections Branch’s “Emergency Policy” for inspections became the “Emergency Off-Site Inspection Policy,” although no off-site inspections were started. |
| March 27 | Ontario Regulation 95/20 came into effect, which allowed long-term care homes to stop documenting some care-related information. |
| April 2020 | |
| April 3 | The Minister of Long-Term Care announced that the “ACTIONline” for complaints was now called the “Family Support and Action Line.” |
| April 16 | In preparation for a return to on-site inspections, the Branch began its efforts to find personal protective equipment (PPE) for inspectors. |
| April 21 | Public Health Ontario delivered online training to the inspectors on infection prevention and control and PPE. |
| April 21 | The Hamilton service area office launched the first off-site inspection since the pandemic started. |
| April 27 – 28 | The Canadian Armed Forces began providing assistance at five long-term care homes at the request of the province. |
| April 29 | The government told the inspectors’ union it would rely on volunteers when inspections resumed. |
| April 30 | The Inspections Branch provided inspectors with PPE. |
| May 2020 | |
| May 8 | The Toronto and Ottawa areas began on-site and off-site inspections. The Inspections Branch Director decided any inspector without an accommodation could be deployed to homes. |
| May 11 – 14 | All seven service area offices began off-site inspections. Four also resumed on-site inspections. |
| May 12 | Ontario Regulation 210/20 went into effect. It gave the Inspections Branch Director broad authority to issue a mandatory management order if there was a single COVID case in a home. |
| May 14 | The Canadian Armed Forces sent a letter to military leadership and federal government officials with observations about the five homes it had been supporting to that point. The Ministry of Long-Term Care did not receive these observations for another 10 days. |
| May 20 | The Minister’s office allowed the Branch to resume issuing inspection reports to homes. No enforcement action had been taken for over two months. The Branch began issuing reports the next day. |
| May 24 | The observations of the Canadian Armed Forces reached the Deputy Minister of Long-Term Care. Ministry officials forwarded them to the Inspections Branch. |
| May 25 | The Branch issued its first COVID-related mandatory management orders, to Downsview Long-Term Care Centre and River Glen Haven Nursing Home. |
| May 28 | The Branch had inspections under way at all five homes supported at that time by the Canadian Armed Forces. |
| June 2020 | |
| June 1 | Ontario Ombudsman Paul Dubé announced this investigation.[163] |
| June 2 | The Inspections Branch Director issued a COVID-related mandatory management order to Forest Heights long-term care home. This was the last mandatory order issued during the first wave. |
| June 4 | The Ministry of Long-Term Care approved the first COVID-related voluntary management contract. Six more were approved during the first wave. |
| June 15 | The Hamilton service area office restarted on-site inspections – the last service area to do so. |
| July 2020 | |
| July 9 – August 26 | The Branch issued its inspection reports regarding the Canadian Armed Forces’ concerns at five homes. |
| July 15 | Long-term care homes were required to resume documenting care-related information. |
| July 29 | The province announced the formation of the independent Long-Term Care COVID-19 Commission. |
Appendix B: Judgement Matrix grid
Note: Codes in the three columns from the right refer to potential actions to address non-compliance. From least to most severe, they are:
- WN = written notification
- VPC = voluntary plan of correction
- CO = compliance order
- WAO = work / activity order
- DR = director’s referral
- FS = “financial sanctions” (order that funding be returned or withheld)
- MMO = mandatory management order
- RL/IM = revoke license / interim manager
The underlined codes indicate the “default” or “median action” for the relevant level of non-compliance. More than one action could be taken for each issue.
Appendix C: New enforcement action decision-making criteria
The Ministry’s new tool for determining the appropriate enforcement action is called the Non-Compliance Decision Making tool. It uses the following decision-making criteria. The inspector determines the severity of the issue (high, moderate or low), then whether it is “isolated” or “not isolated.” Lastly, the inspector must determine whether there was previous non-compliance for the same legislative provision within the last 36 months (“existing” or “none”). Once this information has been added, the tool will direct inspectors to one enforcement action in the right-hand column.
The available enforcement actions (right-hand column) are:
- WN = written notification
- CO = compliance order
- CO (HP) = high priority compliance order. A “high priority” compliance order must usually be implemented in 7-21 business days – a shorter timeframe than other compliance orders.
[1] Consistent data tracking ended in April 2022. The real numbers of deaths and infections are almost certainly higher, as there were undetected infections throughout the pandemic, especially in the earliest weeks of the first wave before large-scale testing was available and prioritized in long-term care.
[2] To protect confidentiality, the names used in this report are pseudonyms, and the gender used for them and their loved ones was randomly chosen. For other people quoted and referred to throughout this report (e.g., Ministry of Long-Term Care inspectors, other officials), we have verified pronouns where possible; in some cases, gendered or non-binary pronouns are randomly chosen, or used to protect the individual’s identity.
[3] Ombudsman Act, RSO 1990, c O.6.
[4] Megan Ogilvie, “We know there will be another pandemic. Here’s what four leading Canadian scientists are doing about it”, Toronto Star (March 27, 2023), online.
[5] Catherine Caruso, “COVID-19’s Lessons for Future Pandemics” (November 17, 2022), online: Harvard Medical School.
[6] Appendix A to this report provides a chronology of how the pandemic affected long-term care through the first wave.
[7] Ontario has a legislated Residents’ Bill of Rights, found in section 3 of both the current and former long-term care homes legislation, see Fixing Long-Term Care Act, 2021, SO 2021, c 39, Sched. 1 [Fixing Long-Term Care Act]; Long-Term Care Homes Act, 2007, SO 2007, c 8 (repealed in April 2022) [Long-Term Care Homes Act].
[8] Memorandum from Dr. David Williams, Chief Medical Officer of Health to Long-Term Care Homes, Retirement Homes, Supportive Housing, Hospices and other congregate care settings (March 13, 2020), online.
[9] Directive # 3 issued under s 77.7 of the Health Protection and Promotion Act, RSO 1990, c H.7 [Health Protection and Promotion Act], from the Chief Medical Officer of Health, David Williams (March 30, 2020) at 4 [March 30 CMOH Directive], online: Ontario Hospitals Association.
[10] A copy of this letter was later published by the media, see Letter from CJJ Mialkowski, Brigadier General (May 14, 2020) in TVO Today, “COVID-19: Read the Canadian Forces report on long-term care” (May 26, 2020) [May 2020 CAF Letter], online: TVO Today.
[11] Ombudsman Ontario, Press Release, “Ombudsman Finds Delays, Inconsistencies and Lack of Transparency in Monitoring of Long-Term Care Homes” (December 21, 2010), online: Ombudsman Ontario.
[12] Letter from André Marin, Ontario Ombudsman to the Legislative Assembly of Ontario (December 21, 2010), online.
[13] For the Long-Term Care COVID-19 Commission’s Final Report and two Interim Reports, see Ontario’s Long-Term Care COVID-19 Commission: Final Report (April 30, 2021) (Chair: the Hon. Frank N. Marrocco) [LTC Commission Final Report], online. For chapters 1-5 of the Office of the Auditor General’s COVID-19 Special Report, see “Special Reports” (last modified May 16, 2023) [“Auditor General Special Reports”], online: Office of the Auditor General of Ontario. For Chapter 6, which is an appendix to the Auditor General’s 2021 annual report, see Office of the Auditor General of Ontario, Value-for-Money Audit: COVID-19 Personal Protective Equipment Supply (December 2021) [“Auditor General Report – Chapter 6”], online. For the Patient Ombudsman’s three Special Reports, see “Special Releases” [“Patient Ombudsman Special Releases”], online: Patient Ombudsman.
[14] The Advocacy Centre for the Elderly is a specialty community legal clinic that was established to provide a range of legal services to low-income seniors in Ontario. The legal services include advice and representation to individual and group clients, public legal education, law reform and community development activities.
[15] LTC Commission Final Report, supra note 13 at 301.
[16] “Explore Your Care Options: Long-term care homes” (last updated August 24, 2022), online: Ministry of Long-Term Care.
[17] The data in this paragraph is taken from the Ministry of Long-Term Care’s 2020 staffing study report: Ontario, Ministry of Long-Term Care, Long-Term Care Staffing Study, prepared by the Long-Term Care Staffing Study Advisory Group (July 30, 2020) at 2 [Long-Term Care Staffing Study], online.
[18] Long-Term Care Homes Act, supra note 7; O Reg 79/10.
[19] The new legislation was accompanied by a new regulation, see Fixing Long-Term Care Act, supra note 7; O Reg 246/22.
[20] Long-Term Care Homes Act, supra note 7, s 95(1); Fixing Long-Term Care Act, supra note 7, s 98(1).
[21] Emergency Management and Civil Protection Act, RSO 1990, c E.9 [Emergency Management and Civil Protection Act]; O Reg 380/04.
[22] Excellent Care for All Act, 2010, SO 2010, c 14, s 13.1(2).
[23] “Frequently Asked Questions: How will you help me?”, online: Patient Ombudsman.
[24] For the Patient Ombudsman’s three COVID-19 Special Reports, see “Patient Ombudsman Special Releases”, supra note 13.
[25] The public health units and their areas are prescribed by RRO 1990, Reg. 553, made under Health Protection and Promotion Act, supra note 9. For a map and list of the public health units, see “Public Health Units”, online: alPHa: Association of Local Public Health Agencies.
[26] Health Protection and Promotion Act, supra note 9, s 27(2)–(3) and O Reg 135/18, s 1, Table, row 18.1.
[27] Ontario, Ministry of Health and Long-Term Care, Institutional/Facility Outbreak Management Protocol, 2018, prepared by the Population and Public Health Division (January 1, 2018), online.
[28] Ibid.
[29] “Ontario Health Plan for an Influenza Pandemic 2013” (August 9, 2018), online: Ministry of Health/Ministry of Long-Term Care.
[30] Ontario Ombudsman, 2020-2021 Annual Report, (June 29, 2021) at 5, online.
[31] The Ombudsman has limited authority to accept complaints about whether meetings of Boards of Health for public health units have complied with the open meeting requirements set out in section 238 and 239 of the Municipal Act, 2001, SO 2001, c 25. See Ontario Ombudsman, 2021-2022 Annual Report, (August 10, 2022) at 56, online.
[32] Ontario, Public Inquiry into the Safety and Security of Residents in the Long-Term Care Homes System: Final Report, vol 1(Toronto, 2019) (Chair: the Hon. Eileen E. Gillese) at 1 [Gillese Inquiry Final Report], online.
[33] Ibid at 9.
[34] Ibid at 11, 14–16.
[35] See Recommendation 62: ibid at 37.
[36] See Recommendations 25–6: ibid at 27.
[37] See Recommendations 27–8: ibid at 27.
[38] See Recommendations 23–4: ibid at 26–7.
[39] See Recommendations 85: ibid at 42.
[40] Long-Term Care Staffing Study, supra note 17 at 28.
[41] The Hon. Frank Marrocco et al, “Statement by the Commissioners”, Update Statement, (July 30, 2020), online: Ontario's Long-Term Care COVID-19 Commission.
[42] Letter from the Hon. Frank N. Marrocco, Chair, Ontario’s Long-Term Care COVID-19 Commission et al to Merrilee Fullerton, Minister of Long-Term Care (October 22, 2020), online.
[43] See Recommendations 1–4: ibid at 2.
[44] See Recommendations 1–2: ibid at 3.
[45] See the recommendations listed under “2. Performance Indicators”: Letter from the Hon. Frank N. Marrocco, Chair, Ontario’s Long-Term Care COVID-19 Commission et al to Merrilee Fullerton, Minister of Long-Term Care (4 December 2020) at 3–4, online.
[46] Ibid at 5.
[47] Ibid at 5–6.
[48] LTC Commission Final Report, supra note 13 at 282–320.
[49] Ibid at 2, 19, 48, 212–215.
[50] Ibid at 95–101.
[51] Ibid at 9–11.
[52] Ibid at 114–124.
[53] Ibid at 285–288.
[54] Ibid at 10, 133–39.
[55] See Recommendations 17–21, ibid at 292–293.
[56] Ibid at 113–114, 123, 142–143, 164–165, 359, 365.
[57] Ibid at 17, 181–182, 234.
[58] Ibid at 60.
[59] See Recommendations 24–8, 51(d), ibid at 5–6, 76–77, 294–296, 305–306 (rec 51(d)).
[60] Ibid at 126.
[61] See Recommendations 9a, 40–48, ibid at 48–65, 215–216, 289, 301–305.
[62] Ibid at 70.
[63] Ibid at 207–08.
[64] See Recommendations 9c, 76–66, ibid at 69–70, 151, 207–208, 289, 316–317.
[65] See Recommendation 78a, ibid at 71–72, 318.
[66] Ibid at 157.
[67] Ibid at 13, 169–171.
[68] The 2015 Auditor General’s report was published before the Ministry of Long-Term Care was established as a ministry separate from the Ministry of Health: Office of the Auditor General of Ontario, Annual Report 2015, ch. 3.09 “Long-term-care Home Quality Inspection Program” (December 2, 2015) at 369, 375, online.
[69] Ibid at 370.
[70] Ibid at 370–71.
[71] See Recommendation 6, ibid at 385.
[72] Office of the Auditor General of Ontario, Annual Report 2017, vol. 2, ch. 1.09 “Long-Term-Care Home Quality Inspection Program: Follow-Up on VFM Section 3.09, 2015 Annual Report” (December 6, 2017) at 119–120, online.
[73] The Auditor General provided a diagram showing the different components of its review in Chapter 5: Office of the Auditor General of Ontario, Special Report on COVID-19 Preparedness and Management: Chapter 5, Pandemic Readiness and Response in Long-Term Care, (April 2021) at 7 [“Auditor General Report – Chapter 5”], online. For chapters 1–5 of the Office of the Auditor General’s COVID-19 Special Report, see “Auditor General Special Reports”, supra note 13. For chapter 6, which is an appendix to the Auditor General’s 2021 annual report, see “Auditor General Report – Chapter 6”, supra note 13.
[74] “Auditor General Report – Chapter 5”, supra note 73 at 7.
[75] Ibid at 5.
[76] Ibid at 10, 53–54, 79–83, 85.
[77] Ibid at 74–76.
[78] The Long-Term Care COVID-19 Commission’s Final Report, discussed above, would later feature very similar to findings to these. See Office of the Auditor General of Ontario, Special Report on COVID-19 Preparedness and Management: Chapter 2, Outbreak Planning and Decision-Making, (November 2020) at 3–7, online.
[79] “Auditor General Report – Chapter 6”, supra note 13 at 2–4.
[80] For Chapters 1, 3 and 4 of the Auditor General’s Special Reports on COVID-19 Preparedness and Management, see “Auditor General Special Reports”, supra note 13.
[81] Patient Ombudsman, News Release, “Patient Ombudsman launches systemic investigation into the resident and caregiver experience at Ontario’s Long-term Care Homes with outbreaks of COVID-19” (June 2, 2020), online.
[82] See “Patient Ombudsman Special Releases”, supra note 13.
[83] Ontario, Patient Ombudsman, Honouring Voices and Experiences: Long-term care home survey, COVID-19 Special Report 3 (December 2021) [“Patient Ombudsman – Special Report 3”], online.
[84] Ontario, Patient Ombudsman, Honouring the voices and experiences of Long-Term Care Home residents, caregivers and staff during the first wave of COVID-19 in Ontario, COVID-19 Special Report 1 (October 2020), online.
[85] Ontario, Patient Ombudsman, Honouring Voices and Experiences: Reflections from waves 2 and 3 of the pandemic, COVID-19 Special Report 2 (August 2021) at 23–28, 34–37, online.
[86] “Patient Ombudsman – Special Report 3”, supra note 83 at 4.
[87] Ibid at 30.
[88] Long-Term Care Homes Act, supra note 7, s 144–148; Fixing Long-Term Care Act, supra note 7, s 147–151.
[89] These are Central West, Central East, Hamilton, London, Ottawa, Sudbury, and Toronto. They are now referred to as “districts”, although this report uses the previous terminology of “service area office” that existed at the time.
[90] Long-Term Care Homes Act, supra note 7, ss 143–144; Fixing Long-Term Care Act, supra note 7, ss 146–147.
[91] “Search for LTC Homes By Home Name”, online: Reports on Long-Term Care Homes.
[92] Long-Term Care Homes Act, supra note 7, ss 152–157. The current legislation contains an amended framework for enforcement actions: Fixing Long-Term Care Act, supra note 7, ss 154–161.
[93] LTC Commission Final Report, supra note 13 at 208.
[94] There have been numerous staffing changes at the Ministry following the first wave of the pandemic. Job titles used in this report refer to the individual who filled the role at the relevant period, unless otherwise specified.
[95] Long-Term Care Homes Act, supra note 7, s 25(1). The current legislation contains the same requirement: Fixing Long-Term Care Act, supra note 7, s 29(1).
[96] Long-Term Care Homes Act, supra note 7, s 25(2).
[97] Fixing Long-Term Care Act, supra note 7, s 29(2).
[98] Ministry of Long-Term Care, News Release, “Ontario Taking Emergency Measures to Support Long-Term Care Homes During COVID-19” (March 28, 2020) [“MLTC March 2020 News Release”], online.
[99] At the time, Local Health Integration Networks were responsible for regional administration of public healthcare services in Ontario. This responsibility now belongs to Ontario Health.
[100] The note for this asterisk (*) and the asterisks for the other levels states: “Note: It may be necessary to consider the risk of harm to the resident(s) in the ‘situation or the operations of the home’ as opposed to the harm it caused the resident.”
[101] These provisions reflect the legislated requirements for immediate inspections: Long-Term Care Homes Act, supra note 7, s 25(2); Fixing Long-Term Care Act, supra note 7, s 29(2).
[102] Dr. Merrilee Fullerton, “Reminder to please share (2/2): By calling in, you will reach one of our many experienced #LTC Inspectors, who can answer questions, help you find solutions, or even just have a chat. They are here to help as we face this ever evolving pandemic. #InThisTogether #OntarioStrong” (April 3, 2020 at 8:40), online Twitter.
[103] The allegations against some long-term care homes and others in this report are unproven and were not inspected or verified by the Ministry of Long-Term Care. The focus of this report is on the Ministry’s response to serious allegations brought forward by the public, not the care provided at individual long-term care homes.
[104] See e.g. Hallie Golden, “Washington nursing home at center of US coronavirus outbreak reports 13 deaths”, The Guardian (March 7, 2020), online; André Picard, “Senior care facilities are especially vulnerable to COVID-19 outbreaks”, The Globe and Mail (March 8, 2020), online; Emilio Parodi, “Uncounted among coronavirus victims, deaths sweep through Italy's nursing homes”, Reuters (March 18, 2020), online.
[105] Long-Term Care Homes Act, supra note 7, s 5. The current legislation contains the same requirement: Fixing Long-Term Care Act, supra note 7, s 5.
[106] This definition is followed by some very specific situations that do not constitute a risk of harm, including such situations as thumb tacks on a cork board, lighters, and knives/gardening tools/knitting needles/buttons in a jar in an open room (such as an activity room).
[107] Long-Term Care Homes Act, supra note 7, s 25(1); Fixing Long-Term Care Act, supra note 7, s 29(1).
[108] Eventually, the matter was inspected.
[109] Directive # 3 prevented most visitors from entering the home for most of the first wave: March 30 CMOH Directive, supra note 9.
[110] The long-term care legislation requires every long-term care home to have a residents' council. The council can advise residents of their rights, and can attempt to resolve disputes between a resident and their home. The council can also report concerns and make recommendations to the home. It can also report concerns to the Director of the Ministry's Inspections Branch. For more, see Long-Term Care Homes Act, supra note 7, ss 56–58; Fixing Long-Term Care Act, supra note 7, ss 62–64.
[111] Long-Term Care Homes Act, supra note 7, s 26; Fixing Long-Term Care Act, supra note 7, s 30. The 2021 legislation includes additional protections for disclosure to the Ministry of Long-Term care personnel or other prescribed individuals or entities. Residents’ Councils and Family Councils are prescribed for this purpose in O Reg 246/22, s 117.
[112] Long-Term Care Homes Act, supra note 7, s 26(1)(d); Fixing Long-Term Care Act, supra note 7, s 30(1)(d).
[113] The Ministry of Labour is responsible for investigating allegations that a workplace, such as a long-term care home, has contravened the Occupational Health and Safety Act, RSO 1990, c O.1.
[114] O Reg 79/10, s 107 (under the former Long-Term Care Homes Act, supra note 7); O Reg 246/22, s 115 (under the current Fixing Long-Term Care Act, supra note 7).
[115] “Auditor General Report – Chapter 5”, supra note 73 at 73.
[116] The Ministry’s list of high-risk homes was constantly changing as homes’ outbreaks began and ended. As a result, the number of high-risk homes that required inspection also changed day-to-day.
[117] O Reg 95/20, ss 3(ii)(A)–(B), as made under the Emergency Management and Civil Protection Act, supra note 21, on March 27, 2020.
[118] O Reg 412/20, s 5(2) revoked s 3(ii) of O Reg 95/20 on July 15, 2020, and long-term care homes were once again required to complete these types of documentation. The provisions of the regulation still in force after this amendment were continued under the Reopening Ontario (A Flexible Response to COVID-19) Act, 2020, SO 2020, c 17 [Reopening Ontario Act] when that Act was proclaimed in force on July 24, 2020.
[119] “MLTC March 2020 News Release”, supra note 98.
[120] “Auditor General Report – Chapter 5”, supra note 73 at 5.
[121] The Ministry of Labour, Immigration, Training and Skills Development enforces occupational health and safety related provisions in various statutes through proactive and complaint-related inspections.
[122] A copy of this letter was later published by the media, see May 2020 CAF Letter, supra note 10.
[123] Office of the Premier, News Release, “Ontario Taking Action at High Risk Long-Term Care Homes” (May 27, 2020), online.
[124] Ontario, Ministry of Long-Term Care, Inspection Report under the Long-Term Care Homes Act, 2007: Altamont Care Community, Inspection No 2020_595110_0009 (July 29, 2020) [“July 2020 Inspection Report – Altamont Care Community”], online.
[125] A pressure ulcer is a lesion caused by unrelieved pressure that results in damage to underlying tissue.
[126] Ontario, Ministry of Long-Term Care, Inspection Report under the Long-Term Care Homes Act, 2007: Hawthorne Place Care Centre, Inspection No 2021_631210_0019 (August 4, 2021) [“Hawthorne Place Inspection Report”], online.
[127] LTC Commission Final Report, supra note 13 at 186.
[128] “Hawthorne Place Inspection Report”, supra note 126 at 5.
[129] Ontario, Ministry of Long-Term Care, Inspection Report under the Long-Term Care Homes Act, 2007: Downsview Long Term Care Centre, Inspection No 2020_816722_0007 (June 4, 2020) at 11, online.
[130] LTC Commission Final Report, supra note 13 at 186.
[131] Ontario, Ministry of Long-Term Care, Inspection Report under the Long-Term Care Homes Act, 2007: Downsview Long Term Care Centre, Inspection No 2021_526645_0011 (A1) (October 22, 2020), online.
[132] The legislation noted that long-term care residents were able to make such reports, but were not required to: Long-Term Care Homes Act, supra note 7, s 24(3). The current legislation contains the same provision: Fixing Long-Term Care Act, supra note 7, s 28(3).
[133] Long-Term Care Homes Act, supra note 7, s 24(1). The current legislation contains the same wording: Fixing Long-Term Care Act, supra note 7, s 28(1).
[134] From April 2022 onwards, where the non-compliance is low-risk, and where the home has remedied it during the inspection, the inspector does not have to issue an enforcement action.
[135] The Fixing Long-Term Care Act, 2021 removed the Voluntary Plan of Correction (VPC) from the list of enforcement actions: Fixing Long-Term Care Act, supra note 7, s 154(1).
[136] Long-Term Care Homes Act, supra note 7, ss 163–170; Fixing Long-Term Care Act, supra note 7, ss 169–176.
[137] Long-Term Care Homes Act, supra note 7, s 50(1), 152(1)(4), 155–157; Fixing Long-Term Care Act, supra note 7, s 56(1), 154(1)(4), 156–159.
[138] Long-Term Care Homes Act, supra note 7, ss 164–170; Fixing Long-Term Care Act, supra note 7, ss 170–176.
[139] Long-Term Care Homes Act, supra note 7, s 162.2, 182; Fixing Long-Term Care Act, supra note 7, s 168, 192.
[140] Long-Term Care Homes Act, supra note 7, s 156.1. This provision was not proclaimed in force before the Act itself was repealed.
[141] Fixing Long-Term Care Act, supra note 7, s 158.
[142] Ontario, Ministry of Long-Term Care, Inspection Report under the Long-Term Care Homes Act, 2007: The Villages at St. Clair, Inspection No 2019_533115_0004 (A1) (April 10, 2019), online. While the public inspection report does not mention any Director referral, internal Ministry documents confirm that the infection prevention and control issues at The Village at St. Clair were referred to the Inspections Branch Director in March 2019.
[143] Ontario, Ministry of Long-Term Care, Inspection Report under the Long-Term Care Homes Act, 2007: Midland Gardens Care Community, Inspection No 2019_780699_0024 (A1) (April 22, 2020), online.
[144] “July 2020 Inspection Report – Altamont Care Community”, supra note 124.
[145] Ontario, Ministry of Long-Term Care, Inspection Report under the Long-Term Care Homes Act, 2007: Altamont Care Community, Inspection No 2020_748653_0020 (November 13, 2020), online.
[146] Ontario, Ministry of Long-Term Care, Inspection Report under the Long-Term Care Homes Act, 2007: Pinecrest Nursing Home (Bobcaygeon), Inspection No 2020_643111_0011 (June 30, 2020), online.
[147] “Hawthorne Place Inspection Report”, supra note 126.
[148] Fixing Long-Term Care Act, supra note 7, ss 154(1), 158; O Reg 246/22, s 349.
[149] O Reg 246/22, s 349(6).
[150] Fixing Long-Term Care Act, supra note 7, s 192.
[151] “Auditor General Report – Chapter 5”, supra note 73 at 74; LTC Commission Final Report, supra note 13 at 71–72.
[152] Fixing Long-Term Care Act, supra note 7, ss 159, 161. Section 159(2) lists the circumstances in which the Ministry may suspend (or revoke) a licence. The list includes the situation where a person is in a position to acquire control of the home, or has gained a controlling interest in the home without the Ministry’s knowledge. Section 159(3) provides for the immediate effect of a suspension upon service of a copy of the order on the licensee.
[153] Long-Term Care Homes Act, supra note 7, ss 157–58; Fixing Long-Term Care Act, supra note 7, ss 159(5)–(10), 160, 161.
[154] O Reg 246/22, s 348.
[155] Fixing Long-Term Care Act, supra note 7, s 154 (2).
[156] Long-Term Care Homes Act, supra note 7, s 156; Fixing Long-Term Care Act, supra note 7, s 157.
[157] Long-Term Care Homes Act, supra note 7, s 156(1).
[158] O Reg 210/20 was originally made under the Emergency Management and Civil Protection Act, supra note 21, and under the Reopening Ontario Act, supra note 118, when that Act was proclaimed in force on July 24, 2020. The Regulation was revoked on March 28, 2022.
[159] Long-Term Care Homes Act, supra note 7, s 110; Fixing Long-Term Care Act, supra note 7, s 113.
[160] Fixing Long-Term Care Act, supra note 7, s 157.
[161] Gillese Inquiry Final Report, supra note 32 at 11, 14–16.
[162] Ombudsman Act, supra note 3.
[163] Ontario Ombudsman, Press Release, “Ontario Ombudsman to Investigate Government’s Oversight of Long-Term Care Homes during Pandemic” (June 1, 2020), online: Ontario Ombudsman.