From Hope to Despair
Investigation into the Ministry of Health and Long-Term Care's refusal to fund the drug Cystagon for treatment of Batten's Disease.
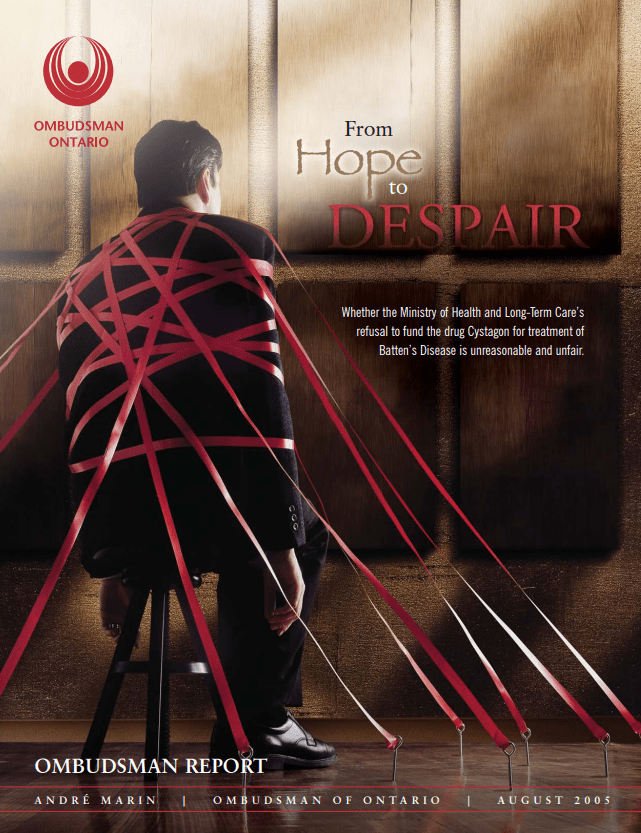
Table of contents
Show
Hide
Investigation into the Ministry of Health and Long-Term Care's refusal to fund the drug Cystagon for treatment of Batten's Disease
"From hope to despair"
André Marin
Ombudsman of Ontario
August 2005
Contributors
Director, Special Ombudsman Response Team (SORT)
- Gareth Jones
Senior Counsel
- Laura Pettigrew
- Wendy Ray
Investigator
- Anne Hart
Executive Summary
1 Christopher Comeau-D’Orsay is gravely ill. When he was diagnosed with a form of Batten’s Disease, a cruel degenerative condition that was destroying his brain, his family was told he was going to die. They would have none of it – not without a fight. He was whisked off to New York to participate in a clinical trial for a new treatment for this rare condition. Within weeks, despair turned to hope. The drug he was being given, Cystagon, was not only stabilizing him, he was getting better. For only $15,000 a year, less than the cost of the futile publicly funded treatments he was receiving in Ontario, he was getting better. The only hitch, and it was a big one, is that his family cannot afford the drug. It is simply beyond their means. But that didn’t matter, they thought. They are blessed. They are from Ontario, a province that prides itself on the medical care it offers its residents. Surely the province would pay for the drug. It would save the Province money if it was to do so, but more importantly, it would save the boy’s life.
2 When the Comeau-D’Orsays applied for support, all hope turned to despair. They were told no. As I write this Report, the Comeau-D’Orsays are mortgaging their future in an effort to give their son one. And even that may not be enough. Without funding they will not be able to go on. As I say, they have been taken from hope to despair. This cannot be allowed to continue. Fortunately, it need not. Christopher Comeau-D’Orsay has been told “no,” without good reason, and for many wrong reasons, and there is still time to get it right.
3 Remarkably Christopher’s plight did not rally this Province’s medical administrators into a committed effort to make it happen; instead his peril received a confused, lethargic and infuriating response, the kind that no resident of this Province should encounter even on small matters. More is the pity, for this is no small matter.
4 A number of things happened that should not have. First, Christopher’s family was told, incorrectly, that their issue was a federal matter even though funding is a provincial matter, and it was fobbed off without explanation to a federal program that has nothing to do with funding. Second, the “law” was invoked to justify the refusal. The family was told that legislation and regulations prohibit the funding they seek, even though the law does no such thing. Third, medical administrators denying the claim have been citing inconsistent government policies, some claiming that funding can only be provided for drugs approved for sale in Canada, with others claiming that funding can be provided even if a drug is not approved for sale so long as the Federal government agrees to provide special access. Medical administrators cannot get their story straight on the basic policies underlying the decision they need to make. Fourth, Christopher’s family was led to believe that the problem was with the drug – that it couldn’t be subsidized in Ontario – even though the Province is paying for that very same drug for other people. Fifth, Christopher was not told about a Provincial program that was set up precisely to help families deal financially with medical conditions like his own, the Inherited Metabolic Diseases (IMD) Program. It took six months before his family learned from the Ministry that the program existed, and when its existence was confirmed by Ministry officials this was not done to facilitate the family’s quest for subsidy. The information was provided in a self-serving attempt by medical administrators to try to explain why the Province was funding others for the same drug and not him. Those others had received approval under the Program, leaving his family to wonder, what about Christopher? Could he get funded under the program? Apparently not – not because his case was unmeritorious but because the program had become so degraded by administrative neglect that it had become moribund – useless. The very program designed to help victims like Christopher and to provide the kind of specialized expertise needed to administer health for such rare and destructive conditions had wasted away because of bureaucratic infighting and lack of commitment. For six months Christopher’s family was not told about the Program he needed because it had imploded, leaving the Province to claim that it could do nothing because its hands were tied. Finally, to add insult to injury, his family was told to throw themselves on the mercy of the pharmaceutical company. Instead of their own Province showing compassion and ensuring the full and proper discharge of its responsibility to consider funding, the family was told to depend on the compassion of a foreign, private, for-profit conglomerate that bore no responsibility to even answer their request. Without doubt, the Comeau-D’Orsays’ quest for funding for their desperately ill child became an exercise in bureaucratic futility, which, after a year and numerous phone calls and letters has still not been properly evaluated. The Ministry of Health and Long-Term Care should be both embarrassed and thankful that it is not yet too late. Christopher’s family is not yet bankrupt and he is not yet dead. I am going to recommend in this Report that Christopher’s treatment be funded – retroactively – that the family’s despair be lessened and that it be given its hope back, but before I do, I need to address head-on the confused policies that are being thrown up as roadblocks.
5 If it is indeed the policy in this Province (relating to any of its discretionary drug subsidy programs) to permit funding only for drugs that have been approved by the Federal Government for sale, that policy should be replaced. It is too narrow - arbitrarily so. Like Christopher, many residents of this Province are taking prescription drugs legally that are not approved for sale. The drugs they take are safe enough or efficacious enough but are not offered for sale simply because they are not profitable to market. What kind of message is that? If a pharmaceutical company can profit in Canada by selling the drugs, we may fund it, otherwise we won’t. This policy prevents subsidy for needed medication, no matter how elderly or poor the claimant is, or how crushing the drug debt is. There is no merit in such a policy. Denying Christopher’s claim without considering his need, the dramatic impact the drug has had for him or the fact that paying for it will save Ontario money simply because the manufacturer does not want to market the drug generally in Canada epitomizes the kind of bureaucratic gridlock that infuriates right-thinking Ontarians, and in this case, threatens the health of one of its most vulnerable citizens.
6 So I am recommending three things in this Report.
First, fund Christopher – retroactively. The drug he requires, Cystagon, is legal for him to receive. It is the only possible treatment. Even though it cannot be scientifically supported because the rarity of his disease inhibits full scientific method from being satisfied, a number of experts affirm that it is the drug that is keeping him alive. His parents are experiencing the kind of crushing drug debt that the Province has undertaken in its drug subsidy programs to relieve. Funding the drug will save the Province money. And there is no reason to let him die in the interests of long-term fiscal restraint or protecting the health of others; the decision will be a discretionary one based on the peculiar facts of his case, and other claims can be dealt with on their own merits. If one considers this claim without unthinking generality or bureaucratic error there is simply no conscionable way to deny it.
7 I am also recommending that if the “approved for sale” policy is indeed currently being applied in Ontario that it be replaced by a policy that would permit subsidy for any drug that is approved for sale or authorized by the Federal government for special access. Whether subsidization would occur in an individual case would be determined on its merits instead of despite its merits.
8 Finally, I am recommending that the Inherited Metabolic Diseases (IMD) Program be reinvigorated without delay, or that an effective successor program be established. This important program deals with the needs of specialized and little understood diseases in an area where, because of research disinterest caused by the rarity of the conditions, there is a lacuna of easily accessible scientific proof. Expert contextual decisions need to be made on the best information available as to how to treat the diseases and what should be subsidized. Do not leave these medical conditions to generalist programs. Christopher Comeau-D’Orsay has been failed because of the neglect of the Inherited Metabolic Diseases (IMD) Program. So have others. In the interests of all of us, fix the thing instead of ignoring it.
“From Hope to Despair”
9 Imagine that you are a parent. One day your healthy seven year old son wakes up. He tries to get out of bed but he cannot walk. You rush him to a doctor who tells you he has a hip infection. They operate but to no avail. His condition worsens. His knees and wrists swell. You are then told he has “reactive arthritis.” He is in pain for more than a year and just as things begin to improve his eyesight starts to fail. He is treated for what is diagnosed as an “immune system reaction,” but his condition worsens. He is becoming progressively blind. You move to a home closer to his school to make things easier, and you do your best to cope as his eyesight diminishes. He turns 15 and then things grow even worse. He begins to hallucinate. He becomes psychotic. Now you are told he has a brain infection. He is given antibiotics but they don’t help. He has a CAT scan and you learn that your son has suffered brain damage. For some reason his neurons have been dying. He is given anti-psychotic drugs and sent home but these drugs don’t work either. He is constantly out of touch with reality. He sleeps only a few hours at a time. You put locks on the door to keep him from wandering outside and you install an alarm system to wake you when he wanders. He begins to lose his ability to walk. Then the doctors get to the bottom of it all. He has an exceedingly rare form of an uncommon disease – Batten’s Disease CLN1, a neurodegenerative disorder. You learn that his disease will take away his ability to walk, talk, and ultimately to eat – that it leads to a feeding tube and to further degeneration. Your son is dying. You are told to put him in a group home because of his advanced dementia and to wait for the disease to take its course.
10 But you will not give up hope. Unable to offer anything resembling a cure, your doctor tells you of a clinical study being undertaken in New York. Since the damage caused by Batten’s Disease can be linked to an abnormal fatty build-up in the brain, doctors there have decided to try treating the condition with a drug, Cystagon, which is used to combat Cystinosis, a disease caused by a similar cellular build-up particularly affecting the kidneys. The doctors have tried fighting Batten’s Disease in a Petri dish with Cystagon and it has worked. You rush to New York with your son and he is accepted into the study and he is given the drug. And then everything changes. Within two months your son’s hallucinations end. His eyesight improves. He begins to walk again. You can have conversations with him, enjoy his company. Tests confirm that the fatty build-up in his brain is now half of what it was. While he is left brain damaged by his ordeal, he is not only alive but functioning well – even able to go back to school. You have found the miracle drug. At $15,000 per year you cannot afford the drug but you thank God you are from Ontario, a province that prizes the health of its residents, a province that has already been subsidizing your son’s health care costs. You have no doubt that the Province will help pay for the drug. After all, it is saving your son’s life and it is cheaper than the care your son required when he was failing.
11 When you contact the Ministry of Health and Long-Term Care to arrange for his drug supply, hope turns to frustration, then despair. You are told that while the government funds other expensive drugs, even for people who have far more money than you do, they do not fund this drug. Even if you go bankrupt and sell your home, not this drug. You are told the law forbids it, that the Provincial government has no choice in the matter because the Federal Government has not approved Cystagon for sale in Canada. It is not a matter where cost considerations or compassion can be allowed any sway. It is the law. It is simply not possible to help you. You are told to see if the drug company will give you the drugs free of charge. Although the words are never spoken, the message is clear - “Even if he were to die as a result, there is nothing we can do. It is out of our hands.”
12 How do you feel when the government rejects you at a time when the price of rejection can mean the life of your son? How much worse do you feel when you learn that much of what the health care administrators have told you is not true; that the Province could fund the drug if it wanted to? It has simply chosen not to because of a general policy that makes no sense in your case and it has failed to help you comply with the requirements that do exist.
13 This account may well be the stuff of nightmares but it is not imagined. It is the story of Christopher Comeau-D’Orsay and his family. At least it is the first few chapters of that story. This Report is intended to improve the end to this story - and it should. To date the Comeau-D’Orsay family has not been given accurate information. Instead they have been given the run-around. They have met with inaccurate excuses, incomplete information and the kind of inertia that has permitted the program that could help save Christopher’s life to atrophy and become dormant. The Comeau-D’Orsay family has been failed by program administrators and policy makers who either do not have an adequate understanding of the rules they administer, or have a lethargy that deprives them of a sufficient sense of what is possible in times of need or of what is needed in times of possibility. Whether Christopher gets his due from the people of this province has nothing to do with the law. It is a matter of choice. This Report is about choosing to help. It is about choosing to help not only the Comeau-D’Orsay family but others who are afflicted not only with this rare and obscene disease but with government maladministration that needlessly compromises their health and, in some cases, may even cost them their lives.
Background
14 I assigned the investigation of Christopher Comeau-D’Orsay’s case to my Special Ombudsman Response Team (SORT). A team of four personnel, including investigators and senior counsel, conducted the investigation.
15 SORT investigators interviewed four officials from the Ministry of Health and Long-Term Care. Two medical specialists also gave generously of their valuable time, providing my investigators with information about Christopher’s situation, as well as, in one case, very candid insights of a practitioner’s view of the Ministry’s programs.
16 The team reviewed over 1000 pages of documentation and interview transcripts. We requested documentation from the Ministry, including briefing notes.
17 All formal interviews were tape-recorded.
18 This Report leads ultimately to the urgent recommendation, among others, that the Comeau-D’Orsay family gets the help it needs.
The Disease and the Miracle Drug
19 Batten’s Disease is a rare condition that affects the body’s cellular waste disposal mechanism, enabling an unhealthy and ultimately devastating build-up of a fatty substance that the body should normally clean away. In the United States, where its frequency has been studied, the disease affects only between 2 and 4 of every 100,000 people. Christopher suffers from a specific form of the disease that plagues only a handful. In his case the disease affects the gene called CLN1. We were advised of only three cases of children suffering from Batten’s Disease CLN1 type in Ontario and of those, only Christopher’s condition is treatable with Cystagon. Batten’s Disease CLN1 is caused by an enzyme deficiency that enables the fatty substance to accumulate, taking its toll on the brain, retina and central nervous system. As Christopher’s case demonstrates, this form of the disease is characterized by blindness, cognitive decline and psychosis. Christopher is currently defying its last manifestations – continued degeneration and death. The general consensus among his doctors is that he is doing so because of Cystagon.
20 It is not even remotely possible to utter any scientific proclamations that Cystagon is the cure for this horrid condition. The lack of scientific proof about how to treat or cure the disease is in large measure because it is mercifully rare. Children afflicted with Batten’s Disease CLN1 frequently die within two to three years, and it is difficult to find children healthy enough to participate in studies. There are not enough subjects to easily achieve scientific proof about drug efficacy. Moreover, the rarity of the disease offers drug companies little incentive to invest in research and development. So no-one can invoke science to declare Cystagon as the cure, and it may be that the small sample sizes will inhibit the ability of anyone to ever make that claim according to scientific standards. There is, however, one thing that all of Christopher’s doctors agree upon and that seems beyond reasonable dispute. For Christopher, the drug is working.
21 It was approximately four years ago that Dr. Minassian, a Pediatric Neurologist at the Hospital for Sick Children, first met Christopher. By that time Christopher had the vision problems and florid psychosis I have described. He was in a wheel chair, incapable of attending school. Dr. Minassian told Christopher’s parents that his condition was terminal. In the absence of any known treatment for the disease, Dr. Minassian referred them to the New York drug study, offering a thin ray of hope. He describes what occurred after Christopher began to receive Cystagon as “remarkable.” He has marveled at Christopher’s “dramatic improvement in a disease that is considered progressive and fatal.” The drug not only arrested the degeneration but Christopher improved. His psychosis is now completely gone. He is now fully able to walk and is able to see shapes. He is back at school learning. He can communicate and is responsive. He is in a stable state. In Dr. Minassian’s opinion, if Christopher hadn’t taken Cystagon he would be dead by now. Dr. Minassian commented on January 21, 2005:
It is completely evident that the medication is working. The [New York] study is still in progress, and will be so for a while, because the disease is rare, and they need more subjects to make definite overall conclusions. However, there is no question that for Christopher, this has been almost a miracle.
22 Dr. Minassian is not the only doctor to conclude that Cystagon is helping Christopher dramatically. Dr. Krystyna Wisniewski, his Pediatric Neurologist in New York, wrote on July 8, 2004 that:
… Since initiation of Cystagon in June 2003, Christopher no longer experiences visual and auditory hallucinations. These hallucinations did not respond to Lithium, Zyprexa, Seroquel, Risperdal and Tegretol. In addition, his cognitive function has remained stable and he is more cooperative and less agitated.
He no longer has seizures. Electron microscopic blood studies show a 50% decrease in cellular storage material.
Christopher has had significant improvements while taking Cystagon. It is imperative that Christopher remains on Cystagon.
23 In a letter dated August 6, 2004, Dr. Elise Heon, Ophthalmologist in Chief, Hospital for Sick Children, wrote:
I feel strongly that Christopher has improved significantly since he has been on Cystagon. I feel that he has recuperated some vision and definitely some visual interaction.… I think it would be of extreme importance that Christopher remains on this medication in order to retain the visual function that he currently has.… When Christopher showed his first severe relapse in 2002, he had almost lost a total light perception. However, now his vision has improved to almost hand motion and he certainly has form perception which allows him to circulate and interact with his environment. I think this improvement is quite spectacular and should be continued.
24 Dr. Kraus, Psychiatrist, wrote on August 20, 2004:
Since initiation of Cystagon in June 2003, Christopher no longer experiences visual and auditory hallucinations. These hallucinations were treatment-resistant to individual and combined treatment trials of lithium olanzapine, quetiapine, risperidone and carbamazephine but have significantly improved with continuing treatment with Cystagon. In addition, his cognitive function has remained stable and he is more cooperative and less agitated. …
Christopher has had significant improvements while taking Cystagon. It is imperative that Christopher remain on Cystagon.
25 While it cannot be predicted that Cystagon will one day be generally accepted as an effective and safe treatment for Batten’s Disease CLN1, the words of Dr. Minassian on that point are apt when it comes to considering Christopher’s needs:
I strongly believe that things should be based on evidence … however we have the proof in the patient himself right now, so we do not need proof from a study…there is nothing better than this kind of proof, because we have the proof from the patient himself, not from groups of other patients…. we have proof that this medication helps this kid and without this medication the kid will die, that is crystal clear for anyone who wants to see it….
26 While “scientific proof” is not available, based on these professional observations one fact is immutable – Cystagon has worked wonders for Christopher Comeau-D’Orsay. It has not only allowed him to experience an improved quality of living, it has kept him alive.
The Cost of Care
27 There is another immutable fact that warrants early introduction. Even leaving aside unquantifiable quality of life considerations, it is far cheaper to give Christopher Cystagon than not to give it to him. The drug, in the dosage that Christopher requires, costs approximately $15,000 per year. It was more expensive when only his symptoms were being treated. Before Cystagon at one point $1,200 per month was being spent on anti-psychotic drugs that were not working, and another $600 per month for food supplements. More significantly, Christopher was on the fast-track to 24 hour a day institutional care, which costs between $90 and $450 a day. In Christopher’s case, Cystagon is not only a life saver, it is also a money saver.
28 Yet Christopher’s family cannot afford the drug. His father, Robert D’Orsay, works as a mechanic. It is difficult for his mother, Wendy Comeau-D’Orsay, to work; in spite of his improvement she still needs to spend her time caring for Christopher. Cystagon is simply beyond their means. Robert D’Orsay’s valiant attempts to fund Cystagon for Christopher are ruining the family financially. His line of credit is “maxed out.” He has logged as much overtime as he can find. His Registered Retirement Savings Plans are gone. All that is left is the family home. The Comeau-D’Orsay family says that next year that too must go. Wendy Comeau-D’Orsay is adamant “we’re not going to take the medicine from him, we have to get the equity out of the house and rent or do something…” They have to mortgage their future to give their son one, and without help, even that will not be enough.
29 Unhindered by rigid rules, binding regulations, or an unthinking commitment to line drawing policies based on generalized fiscal concerns that do not apply in this case, what would the sensible outcome be? The answer is obvious – clear – incontrovertible. The Province of Ontario should be paying for the drug. It is cost effective and human decency requires it. The ultimate question is whether that sensible outcome is possible, or is it to be foiled by rigid rules and binding regulations. The Comeau-D’Orsay family has been told that it is not possible, that the Province’s hands are tied. They have been told this with breathtaking inefficiency even though it is wrong.
Errors, Excuses and Omissions: Roadblocks to Help
30 What the Comeau-D’Orsays encountered when they turned to their government is the kind of malfunctioning bureaucracy that no resident of this Province should ever encounter, even on small issues. More is the pity because the Comeau-D’Orsays’ issue is decidedly not small. Theirs is the kind of plight that one would think would inspire caring individuals to explore the art of the possible rather than passing the matter off as beyond their control. When the Comeau-D’Orsays approached the Premier’s Office, they were told that Christopher’s situation didn’t fit under any Ministry programs and they wouldn’t be receiving any funding. A closer look shows that Christopher could indeed fit the programs if only responsible officials had given him adequate guidance, or nurtured the programs that were in place.
31 In order to describe effectively the problems this family has encountered, it is first necessary to take an admittedly dry but mercifully brief tour through the rules and regulations that relate to the supply of drugs in Ontario.
The Medical Care Complex
32 Anyone rehearsed in the supply of medical services in Canada is aware that, as a federal state, both the provinces and the federal government have a role to play. In simplified terms, the Federal government determines legal access to a drug while the provinces are responsible for delivery and funding.
Access to Drugs – The Federal Role
33 My investigators were advised of three relevant modes of gaining access to drugs in Canada, (1) drugs that have been approved for sale by Health Canada, (2) drugs that have been approved by Health Canada under its Special Access Program, and (3) through a “personal use exemption.” A few words on each of these three methods will be useful.
(1) Access to Approved Drugs
34 A drug can be brought into Canada and distributed if it has been approved by Health Canada to be sold for the treatment of specified conditions. Appropriately, Health Canada imposes exacting, science-based, quality control standards before approving the general marketing of drugs. The Health Products and Food Branch at Health Canada studies both efficacy and safety and decides whether to permit the product to be marketed. Before an approved product can be offered for sale in Canada, Health Canada will issue a Notice of Compliance [NOC] and a Drug Identification Number [DIN]. It generally takes a minimum of one year to obtain a Notice of Compliance, but it can take as long as 10 years.
(2) Access through the Special Access Programme
35 Health Canada’s Special Access Programme permits unapproved drugs to be distributed for a specific person for a defined medical condition. Access through this program is provided on a compassionate or emergency basis to patients with serious or life-threatening conditions when conventional therapies are unsuccessful, unavailable or unsuitable. A medical practitioner will initiate the request for use of the drug. It is that medical practitioner rather than Health Canada who undertakes the risk/benefit decision. Access under the Special Access Programme does not therefore constitute an opinion or statement that the drug is safe, efficacious or of high quality. It is a discrete decision based on circumstantial necessity. Health Canada attempts to process special access requests within 24 hours of receipt. When a drug has been approved under the Special Access Programme the manufacturer is not compelled to furnish it and is free to impose conditions on its supply. While there is no requirement that manufacturers provide drugs free of charge that are approved for Special Access Programme, over the years many have done so.
(3) “Personal Use Exemptions"
36 Section A.01.040 of the Federal Food and Drug Regulation provides:
Subject to section A.01.044, no person shall import into Canada for sale a food or drug the sale of which in Canada would constitute a violation of the Act or the Regulations.
37 This section does not apply if an individual imports a drug for personal use, and not for sale. There are, of course, other provisions making the importation or possession of specified drugs illegal, but so long as a drug is not caught by such provisions and is not brought in for sale, it can be imported lawfully.
Christopher’s Access to Cystagon
38 Cystagon has never been approved for sale in Canada, although it was approved by the U.S. Federal Drug Administration (FDA) for sale in the United States on August 15, 1994. Even though it is being used in Canada to treat fifty or so Cystinosis patients, the company manufacturing the drug is unlikely to market it here. It would not be worth the company’s cost of trying to meet the rigorous standards applied by Health Canada for approving a drug for sale. It would simply not be commercially viable to do so. The drug is made available for use by the Cystinosis patients, however, under the Special Access Programme. No requests for Cystagon for use in Batten’s Disease have ever been made through the Special Access Programme. Christopher’s family has never had to make that application to get Christopher access. He is receiving legal access to the drug under the third mechanism listed. The non-prohibited drug Cystagon is purchased for him from a Pittsburgh pharmacy and imported not for sale, but for his own personal use. Christopher’s current problem is not access. It is funding.
Funding for Drugs – The Provincial Role
39 It is the provincial governments that determine levels of public funding for the prescription drugs required by their residents. Funding for prescription drugs in Ontario is administered by the Ministry of Health and Long-Term Care, under the authority of the Ontario Drug Benefit Act and its regulations. Only drugs prescribed by a member of the health profession licenced to practice in Ontario are eligible for reimbursement. As a result of a series of legal rules this means that a drug must be dispensed in this Province before it can be subsidized. In addition, there are two general requirements for funding under any of the Province’s programs, the first relating to the eligibility of the applicant and the second relating to the eligibility of the drug. The two Ontario programs[1] that are relevant to this Report and their requirements are as follows:
(1) The Trillium Drug Program
40 “Eligible persons” under the Trillium Drug Program[2] are those who have high drug costs relative to their family income. The program is not confined to those who are poor although a deductible is paid based on income and family size. Christopher Comeau-D’Orsay is an “eligible person” under this program.
41 It is not enough to be an “eligible person” in order to receive subsidy, however. The particular drug must be eligible, and not all prescription drugs that are approved for sale or use in Canada qualify. A drug will be eligible if it is listed as a “designated drug” on a list compiled under the regulations to the statute. The list is known as the Ontario Drug Benefit (ODB) Formulary/ Comparative Drug Index. It is compiled by an expert advisory committee, the Drug Quality and Therapeutics Committee, which reviews submissions from manufacturers and makes recommendations to the Minister. Cystagon is not a listed drug. The Comeau-D’Orsays cannot therefore rely on the “designated drug” qualification to receive funding, even if the drug was purchased by them in Ontario.
42 In addition to the designated drug category, there is also special provision made for funding drugs that are not designated. Funding for non-designated drugs is provided for in section 8 of the Ontario Drug Benefit Act, which empowers the Minister to fund unlisted drugs required for the proper treatment of an eligible patient. The Drug Quality and Therapeutic Committee gives the Minister advice on the approval of section 8 applications. If Christopher were to qualify under the Trillium Drug Program, it would have to be through section 8, which is incorporated by regulation into that program.
(2) The Inherited Metabolic Diseases Program
43 There is another program in the Ministry’s arsenal, relevant to this case, to assist Ontarians. It is the Inherited Metabolic Diseases Program (the IMD Program), and it is run by the Public Health Division. The IMD Program is relevant because Batten’s Disease is a metabolic disease. Christopher would therefore be an eligible person under this program.
44 In order to receive financial support under the IMD program, the drug or supplement or special food must be listed as available for the relevant medical condition. The list of approved therapies was developed by an Advisory Committee on Inherited Metabolic Diseases made up of experts from five regional treatment centres. Cystagon is found on the IMD Program list, but it is free only as a treatment for Cystinosis. For reasons that will be discussed below, the Committee has never considered whether Cystagon should be approved for the treatment of Batten’s Disease.
Seeking Funding – An Exercise in Bureaucratic Futility
45 It was through this complex of regimes and programs that Robert D’Orsay had to navigate in his quest to obtain financial support. In the fall of 2004, he was advised by his MPP to apply to the Trillium Drug Program for funding. He submitted his application but was told it would take months to determine whether the Plan would cover the drug under section 8 of the Ontario Drug Benefit Act. Because of the urgency of the matter, on October 27, 2004 Mr. D’Orsay wrote to the Minister of Health, the Honourable George Smitherman, requesting funding. In order to impress the urgency of the matter on the Minister he said he would be forced to go to the media if the matter was not resolved within three weeks.
46 Mr. D’Orsay’s letter, with supporting material, was referred by the Minister’s Office to the Director, Drug Programs Branch, of the Ministry of Health and Long-Term Care. She responded less than 10 days later on November 5, 2004. The letter signed by her, prepared with the assistance of medical administrators in the Ministry, said in relevant part:
Before an unlisted drug can be considered for reimbursement under the ODB program, it must be assigned a Notice of Compliance (NOC) and a Drug Identification Number (DIN) by Health Canada’s Therapeutic Products Program (TPP). The TPP is responsible for approving a drug for sale and marketing in Canada by evaluating its product’s safety and efficacy, and by looking at a large volume of research including animal efficacy and toxicology studies. Once the federal government approves a drug, a NOC and a DIN for the product are issued and the new product can be sold and used widely by physicians in Canada.
Under current legislation governing the administration of the [Ontario Drug Benefit] program, only those drug products that have been approved by Health Canada (i.e., drugs that have been issued a [Notice of Compliance] and a [Drug Identification Number]) can be considered for reimbursement under the [Ontario Drug Benefit] program. As a result, drugs like Cystagon that do not have a [Notice of Compliance] or [Drug Identification Number], are not eligible for listing in the Formulary, or reimbursement under the [Ontario Drug Benefit] program.
As you are aware, a supply of a drug that has not yet been approved by Health Canada can be accessed by physicians on a case-by-case basis through Health Canada’s Special Access Program…. I understand from your letter that Health Canada will only approve Cystagon under its Special Access Program for the treatment of Cystinosis.[3] Unfortunately, given the above, this matter falls under federal jurisdiction, and as such, I would recommend that your son’s physician continue to work with Health Canada and/or the manufacturer of Cystagon to see if supplies could be obtained on a compassionate basis in your son’s particular case.
47 The Director’s letter of November 5, 2004 is not without its ambiguity, but the overall message was clear enough. To a layperson it was a long, complex “no.”
48 Although this letter is not the only communiqué that I am going to take to task, and I do not wish to single it out for particular criticism, I find it convenient to use this letter of November 5, 2004 as a way to organize the more general comments I have about the way the Ministry responded to the Comeau-D’Orsay request.
49 Altogether apart from the ultimate answer, I find this letter to be distressing in a number of specific ways. First, it passes the buck to the Federal Government by telling Mr. D’Orsay to apply to Canada’s Special Access Programme; second, it claims inaccurately that the law requires a drug to be approved for sale in order to be eligible for reimbursement when the law imposes no such requirement; third, taken along with other correspondence, memos and emails it reflects a confusion within the Ministry about what kind of Federal access approvals are required according to its own policies; fourth, it represents inaccurately that Cystagon as a drug cannot be funded; fifth, it fails to disclose the existence and condition of the Inherited Metabolic Diseases (IMD) Program, the program that should provide an alternative source of funding, and sixth, it passes the buck to the pharmaceutical companies without adequate explanation and support. I review each of these six concerns in more detail immediately below. Before doing so I need to deal with one other matter, namely the irrelevance of the Ontario pharmacy notice the family was given.
The Irrelevance of the Ontario Pharmacy Notice
50 Within a few days of receiving the letter of November 5, 2004 from the Director, Drug Programs Branch, and independent of it, Robert D’Orsay was told by administrators in the Trillium Drug Program that his application was denied, and he subsequently received written confirmation of that. The reasons offered by the Trillium Drug Program administrators differed from those in the Director’s letter. The Trillium Drug Program administrators advised Robert D’Orsay in a standard form document that drugs must be dispensed in Ontario to be eligible for benefits under the Trillium Drug Program. I mention this because, taken in isolation, notice of what I have called for convenience the “Ontario pharmacy notice” requirement may cause some to discount his complaint to my Office on the basis either that his claim was not legally eligible whatever else happened, or by concluding that instead of complaining the Comeau-D’Orsays should have searched for a way to get the drugs dispensed in Ontario. In my opinion drawing either of these conclusions would be profoundly unfair. First, the Director’s letter and other things he was told carried the unmistakable message that even if the drug were dispensed in Ontario, Cystagon would not be covered. Why would he try pointlessly to arrange to get a drug from an Ontario pharmacy that he was already obtaining in New York if it would not advance his effort to get the cost subsidized? Second, as the following discussion makes clear, Robert D’Orsay was never given clear guidance on how to make that happen. Although he was told about the Federal Special Access Programme that would have made an Ontario prescription possible, it was never explained adequately to him what use his application to the Federal Special Access Programme would have been. He was never advised that it was a means to an Ontario prescription. In the circumstances, it would be unfair to permit the Ontario pharmacy notice he received to prejudice the Comeau-D’Orsay claim.
51 In any event, that one clear communication hardly eradicates the other problems the Director’s letter of November 5, 2004 epitomizes.
Six Troubling Things
(1) Passing the Buck to the Federal Government
52 Even though Mr. D’Orsay was asking for funding, the last paragraph of the November 5, 2004 letter refers him to the Federal Special Access Programme. This is puzzling without further explanation because that program provides for legal access to drugs, not their funding. It is not clear from the letter why a man who was seeking funding, a matter of Provincial responsibility, was referred to the Federal Program. One possibility-– that the Director, Drug Programs Branch, mistakenly thought that Mr. D’Orsay’s basic problem was access and not funding[4] - can be quickly dismissed. The Director’s own letter of November 5, 2004 opens, “Thank you for your letter about coverage of Cystagon under the Ontario Drug Benefit (ODB) program for your son, Christopher Comeau-D’Orsay.”
53 A second possibility – that Robert D’Orsay was being encouraged to use the Federal Special Access Programme as an avenue for the Provincial government to ultimately approve his funding for the drug, either to remedy the fact that the drugs had to be dispensed in Ontario or on some other basis – is equally unlikely since the Director’s letter makes it clear that funding is available in her opinion only for those drugs that have been fully approved for sale in Canada. She never suggests that drugs authorized federally for special access can be reimbursed by the Province, and there is absolutely no mention made of using Special Access authorization as an avenue for provincial funding.
54 Then there is the startling possibility that at the time the November 5, 2004 letter was written, the Director of the Drug Programs Branch and her staff were confused about the Federal Government’s role, and therefore the Province’s own role, in the supply of drugs. This is suggested by the Director’s curious comment in the letter of November 5, 2004, “Unfortunately, given the above, the matter falls under federal jurisdiction.” The “matter” being discussed was funding and that matter falls under provincial, not federal jurisdiction.
55 I am loath to conclude that there was such a basic misunderstanding within the Provincial government about its own role in the drug supply. I suspect that there is some unexplained point in the reference to the Federal Program. What is clear is that the response represents a woeful failure to communicate effectively. In the end, Mr. D’Orsay was left with the only impression he could have been. When Robert D’Orsay received the Ministry’s letter he realized that it was, in his own words, trying to “put him off to the Feds.” His province, dealing with a man whose urgent and painful problem fell within their bailiwick, was passing him off to another government.
56 This was not the last time he was passed off without adequate explanation to the Federal Government. Six months later, on April 29, 2005, he was again referred by the Director, Drug Programs Branch, to the Federal Special Access Program, only this time she cautioned him: “It should be noted, however, that funding is not provided through this program.”
57 Needless to say, the complex of federal and provincial programs is daunting, even for lawyers and medical administrators. It is regrettable that Mr. D’Orsay was not given a clear explanation as to why the Federal referral was being made. The impression that was left was that while his son’s future was hanging in the balance, he was being given the run-around.
(2) Relying on the “Law” to Deny a Legal Claim
58 I am also deeply troubled that the letter of November 5, 2004 incorrectly tells the Comeau-D’Orsay family that the “law” prohibits the Government from helping them, when it does not. While it is true that there is no legal provision for reimbursement of a New York prescription, the “law” does provide a way for the Comeau-D’Orsays to obtain an Ontario prescription, namely under the Special Access Programme. In any event, the “law” that he was being told impeded his claim is not the Ontario pharmacy requirement. Robert D’Orsay was told “current legislation” only permits Ontario to reimburse residents for drugs that are approved for sale and distribution by the Federal Government, which is not so.
59 It is not only the Director of the Drug Programs Branch who invoked the “law” to justify the refusal of funding. When, on August 5, 2005, Ron Sapsford, the Deputy Minister, responded to my Notice of Intent to investigate, he too expressly invoked the law:
… Cystagon has not been approved for marketing in Canada by Health Canada (i.e. it does not have a NOC or DIN) and therefore, regulations under the Ontario Drug Benefit Act that govern the Ontario’s drug benefit programs prohibit the ministry’s consideration of the funding. (emphasis added)
60 It appears that even the Minister has been briefed that the law ties his hands. On July 21, 2005 a CBC News Report about Christopher’s case quotes the Minister as explaining, “In fact the drug has not been approved by Health Canada and in the absence of an approval from Health Canada we’re not even in a position to cover it.”
61 “It is against the law,” is, of course, a complete answer to any request. An examination of the relevant legal rules shows that it was simply inaccurate to tell both the Comeau-D’Orsays and us that the law prohibits funding Christopher’s care. This is not a case of “we can’t.” It is a case of “we won’t” that has been dressed up like a case of “we can’t.”
62 First, there is no federal law that bears on the matter. The Health Canada officials we contacted were aware of nothing that would prevent a province from funding the drug for Christopher. We have researched the matter on our own and found no such prohibition on provincial funding for legal drugs like Cystagon.[5] Indeed, I am advised by legal counsel that it would be ultra vires or beyond the competence of the Federal Government to tell a province when it can fund drugs that are legally used and when it cannot.
63 What then of provincial law and the Ontario Drug Benefit Act that the Deputy Minister cites? It is important to bear in mind that the Act deals with both “listed drugs” and “unlisted drugs.” In a nutshell, if a drug is not listed as approved for sale, it cannot be funded as a listed drug, but this is simply not so for unlisted drugs. The Province can fund them, whether approved for sale or not. I will deal with “listed drugs” first.
64 Drugs found on the Ontario Drug Benefit (ODB) Formulary/Comparative Drug Index have to be approved for sale by Health Canada in order to be reimbursed, but only because a drug will not be approved for the list unless it is approved for sale. Under regulation 12(1) of O/Reg 201/96 the Province has made Federal sale approval a legal requirement of the Provincial list. Put simply, it is not possible to get reimbursed for a listed drug that has not been approved for sale by Health Canada because no drugs that have not been approved by Health Canada ever make it onto the list. In essence, it is correct, albeit indirectly so, to say oflisted drugs that the law prohibits reimbursement unless they have been approved by Health Canada for sale.
65 What then of “non-listed” drugs like Cystagon? As indicated, provision is made for reimbursement of non-listed drugs under section 8 of the Act. It says:
8(1) If a physician informs the Minister that the proper treatment of a patient who is an eligible person requires the administration of a drug for which there is not a listed drug product, the Minister may make this Act apply in respect of the supplying of that drug as if it were a listed drug by so notifying the physician.
66 When Christopher’s Psychiatrist applied for consideration of Cystagon under the section 8 process, he received a response dated November 10, 2004 advising that the legislation limits the Ontario Drug Benefit Program coverage to pharmaceuticals with a Drug Identification Number.
67 The Trillium Drug Program permits reimbursement for any drugs approved under section 8, and there are no requirements in the Regulations governing that program that confine reimbursement to drugs that have been approved federally for sale.
68 Why would this be so? Why would the Province require listed drugs to be approved for sale by the Federal Government, but impose no similar legal requirement on the reimbursement of non-listed drugs? The answer is obvious. Drugs that are listed are approved generally for reimbursement. There is no case-by-case examination – no opportunity to assess the efficacy or safety for each claim. On the other hand, for drugs not listed for reimbursement, there is a case-by-case assessment that gets done for each application for funding under section 8. The efficacy and safety of the drug can be considered in light of the unique needs of the particular patient. Since there is no pre-approval for reimbursement for non-listed drugs and total control by decision-makers on a case-by-case basis, insisting on prior Federal sale approval would make no sense.
69 The wisdom of the dichotomous approach to “listed” and “unlisted” drugs is, however, not at the centre of the current inquiry. The crucial point is that as a matter of law the Minister and therefore the Ministry has the discretion to pay reimbursement for any legal drugs it wants to under the Trillium Drug Program or any other discretionary funding program.
70 Given the recommendations I am going to make, it is also worth noting that the Minister has the power to approve reimbursement for drugs not approved for sale, altogether apart from the provisions of the Ontario Drug Benefit Act and its Regulations. Even outside of statute the Minister ultimately has the inherent discretion to make funding decisions to promote the health and well-being of the people of Ontario. In a previous investigation undertaken by this Office, the Ministry of Health justified the expenditure of public funds outside of the Ontario Health Insurance Plan on this footing. The Ministry paid, on an emergency basis, for treatment outside the country to assist a 17-year-old girl suffering from environmental sensitivities. This payment was not pursuant to any specific legislative authority or program guideline. In a letter dated October 30, 1997 Legal Counsel for the Ministry explained:
… I can confirm that counsel in the Ministry’s Legal Services Branch share the view that the Minister, generally speaking, does not need specific legislative authority in order to spend public funds. If funds have been appropriated by the Legislature pursuant to the Supply Act, the Minister has the power to spend provided that his or her power to spend has not been, or is not, restricted by statute.
71 In a letter of May 31, 1999, the Acting Director of the Health Services Division stated:
The decision … was not a routine exercise of ministerial discretion made within the framework of an established program for making such decisions.
72 Although this is an authority that, for political and practical purposes, has to be used sparingly, only in the most exceptional of cases, the Minister can decide to fund Cystagon for Christopher outside of the framework of the Ontario Drug Benefits Act. If the Ministry is refusing to fund legally acquired drugs that are not approved for sale by the Federal Government this is a matter of policy, not law. Telling the Comeau-D’Orsays that payment was prohibited by legislation or regulations unless the drugs were approved federally for sale was therefore misleading and inaccurate.
73 I make no finding that these were intentional misrepresentations. Indeed, I am certain they were not. As I say, the law is confusing and mistakes get made. Having said that, one would nonetheless hope that at the most senior levels of government on such an important life-affecting matter that administrators would take the time to get the law right – that they would know the reach of their own rules before deciding – but here they did not. This is more than regrettable. Funding has been peremptorily denied in this case for the wrong reason.
(3) Confusion about Polic
74 What, then, of the “policy” not to fund drugs that are not approved federally for sale? This investigation has left me unsure of whether this even is Ministry policy. We have encountered at least two competing views. First, there is the “approved for sale” policy position that I have just described. Its adherents consider drugs that are not approved by Health Canada for sale to be ineligible for reimbursement. Application of this policy would mean that there could be no reimbursement for prescriptions that have been approved under the Federal Government’s Special Access Programme. The competing view that we encountered, the “approved for sale or special access” position, would allow reimbursement if a drug is approved federally either for sale or underthe Federal Government’s Special Access Programme.
75 From the outset the Comeau-D’Orsays met with administrators who held fast to the “approved for sale” view. Since Cystagon has never been approved for sale, these people took the position that the family was not eligible for reimbursement. This reason for refusal was voiced from time to time with some variation. Most often the family was simply told that there can be no reimbursement unless a drug has been approved for sale but at other times they were told that to be eligible for reimbursement a drug must be assigned a Drug Identification Number (DIN) or that a Notice of Compliance (NOC) must be issued. Admittedly, apart from adding to the confusion, the variety of ways in which the message was delivered did not matter in this case. Cystagon does not have a Drug Identification Number (DIN) or a Notice of Compliance (NOC) and has never been approved for sale; it would have failed eligibility for reimbursement under any of the stated criteria. There are cases, however, where the outcome of a reimbursement application would differ depending upon whether the Ministry applies a DIN policy, a NOC policy, or an “approved for sale” standard. This is because Health Canada does issue NOCs on occasion before DINs, and before final sale approval. It does so in order to enable manufacturers to begin labeling and marketing preparation in advance of final sale approval for drugs that have completed all streams of review. Precision in articulating and applying the policy can therefore matter, so I mention it even though not much turns on it for this case. The essential point is that versions of the “approved for sale” policy have been at the heart of most of the responses the Comeau-D’Orsays have received.
76 This is what the Director of the Drug Programs Branch said in her initial rejection letter of November 5, 2004:
Before an unlisted drug can be considered for reimbursement under the ODB program, it must be assigned a Notice of Compliance (NOC) and a Drug Identification Number (DIN) by Health Canada’s Therapeutic Program (TPP).
77 This same general explanation was offered when Christopher’s section 8 application was refused later in November 2004, and again when the Director wrote to Mr. D’Orsay a second time on April 29, 2005 to affirm the denial of the family’s claim. We also found a number of internal Ministry materials asserting the “approved for sale” policy to be the Ministry’s position, including documents circulated in December 2004 in order to brief staff on what to say to the Comeau-D’Orsays’ MPP when he came to lobby on their behalf (“the Section 8 request for Cystagon for this patient was not approved because it is a Special Access drug and does not have a DIN”). We also encountered the “approved for sale” policy in interviews or documents prepared in response to my Notice of Intent to Investigate. For example, the Assistant Director of the Ontario Drug Benefit program, Brenda Kritzer, took this position in a conversation we had with her on July 11, 2005. She said unless a drug is approved for sale throughout Canada the Ministry of Health and Long-Term Care would not refund any costs to Ontario residents who purchase it. And on July 21, 2005, after we interviewed the Director, Drug Programs Branch, we received a Ministry note, approved by her, which affirmed that this was the relevant policy:
It has always been DPB policy that requests for drug coverage, that have not been issued a NOC, are not considered for reimbursement under the Section 8 mechanism.
78 If the policy is indeed to approve requests for drug coverage only where drugs have been approved for sale then that policy has been lost on others within the Ministry. Notes summarizing a July 21, 2005 “MO” meeting record that those medical administrators in attendance believe that funding is possible for drugs approved under the Special Access Program, even if not approved for sale. They see the policy as an “approved for sale or special access” position. And then there is the Deputy Minister’s response to our investigation. In spite of appearing to insist on full federal sale approval in other places in his response Mr. Sapsford said:
In the absence of a valid NOC, or without approval through Health Canada’s SAP, [Special Access Programme] the ministry is unable to consider funding Cystagon for the treatment of Batten’s Disease (emphasis added).
79 He provided this comment three times, repeating it with respect to each of the Ministry’s relevant funding programs. This can only be taken to mean that the Ministry considers itself free to fund a drug that has been approved for use under Health Canada’s Special Access Program, even if it was never been approved for sale and never given a NOC or a DIN.
80 Then there is the Inherited Metabolic Diseases (IMD) Program. Ministry documents show that the Ministry funds drugs that have never been approved for sale by Health Canada. There are a number of drugs on its list of funded treatments that have never been given that approval, but have been approved for special access. A background briefing note prepared by Dr. Sandra Bennett to assist the Ministry in responding to our investigation records with respect to the IMD program:
“Several things with no NOC and a number of others with no DIN or PIN have been covered for some years now.”
81 Indeed, the Ontario Ministry of Health and Long-Term Care is even paying for the very drug in question, Cystagon, for a number of Cystinosis patients in spite of the fact that Health Canada has never even been asked to approve the drug for sale. If a policy to fund only drugs approved for sale in Canada exists, it is one that is not well known within the Ministry.
82 So I am left unsure. Is the “approved for sale” policy applicable at all, or only under some programs but not others? It is always troubling to encounter policy confusion. Policy confusion can mean the inconsistent application of rules and the improper disposition of eligibility claims. On a matter as important as reimbursement for essential medical treatment, it is reasonable to expect that the Ministry would be able to keep its own policies straight. This is of particular relevance in Christopher’s case. If the “approved for sale or special access” policy is indeed the correct one the family should have been told directly to get Special Access Programme authorization from the Federal government and to then come back for section 8 approval. Instead, the family was made to understand that special access would make no difference; without sale approval, which falls to the manufacturer and not them to secure, no funding could be forthcoming.
(4) Saying Cystagon Cannot be Funded
83 I am troubled that when reimbursement was initially denied in the Director’s letter of November 5, 2004, the Comeau-D’Orsay family was given to believe that the drug, Cystagon, was not eligible for provincial funding, when it was in fact being paid to treat Cystinosis patients. What the letter said, in particular, is that “drugs like Cystagon that do not have a NOC or DIN are not eligible for listing in the Formulary, or reimbursement under the ODB program.” This passage creates the clear misimpression that the province could not fund the drug and that the problem was with the drug itself.[6]
84 I understand that drugs are approved to treat specific medical conditions and that the fact that Cystagon is funded for Cystinosis does not necessarily mean that it would be funded for Batten’s Disease. Yet the dulled and misleading message given to the family that the drug cannot be subsidized has added to the emotional suffering it is enduring. Imagine the frustration when the Comeau-D’Orsays learned that the Government of Ontario was in fact paying for others to have the same drug their son needed and that they were told is ineligible. Any trust they had in the Ministry would be shattered.
85 It was not easy for the Comeau-D’Orsays to discover the truth. When, after receiving the rejection letter, Robert D’Orsay told Christopher’s doctors that the drug Cystagon was not eligible for provincial funding, he was told this was wrong. The doctors advised him that Cystagon was in fact being supplied in Ontario hospitals free to Cystinosis patients. This sent Mr. D’Orsay on a wild goose chase. He called the Ministry again to find out what was going on and was told that the Ministry had no idea how the hospitals were getting the drug. No-one undertook to look into it and get back to him and he was offered no explanation. So Robert D’Orsay called the drug manufacturer. He was told that the company sells the drug in Canada to hospitals to treat approximately 50 Cystinosis patients. When we followed this up we confirmed this, and learned that Cystagon for the treatment of Cystinosis is being paid for by the Province of Ontario. Four Ontario hospitals dispense the drug to a total of 26 patients at a total cost of approximately $87,200.00. Staff at the Hospital for Sick Children confirmed that Cystagon is purchased at wholesale price, dispensed through hospital pharmacies with a 10% markup and an $11.99 per prescription fee, and then paid for by the Ministry of Health and Long-Term Care.
86 The full truth, that Cystagon is eligible for reimbursement for another condition but not for Christopher’s, remains more than a little awkward for those trying to persuade the Comeau-D’Orsays that the Ministry can do nothing. In April when staff was preparing the Director’s ultimate letter of refusal, an internal memorandum was circulated to Dr. Sandra Bennett. It says:
Sandy, Let me know if there is more to offer – The only sticking point for me personally is suggesting on the one hand the HC has not issued a NOC, but on the other hand it is offered for another condition –cystanosis. Let me know if you have any suggested language to soften that message.
87 I understand the discomfort expressed in this memo. Given the demonstrated effectiveness of the drug in treating Christopher, it is hard to explain why it would be funded for others but not for him. I must say, however, that while I understand the unease expressed in the memo I dislike the sentiment underlying the memo. It reflects, in my view, the wrong mission. Instead of asking, “Given that Cystagon is already approved for Cystinosis and is therefore not a drug that is considered too endemically dangerous to proscribe, what, if anything can we do to help the Comeau-D’Orsays obtain funding for this promising treatment for their son’s horrendous condition?,” it asks, “How can we justify not funding them when we fund it for others?”
88 In the end, the language that was chosen to “soften th[e] message” that the Government was in fact funding others who were receiving the drug did anything but. The letter of April 29, 2005 said:
Through the Inherited Metabolic Diseases Program, the ministry’s Public Health Division provides funding for a limited number of drugs, supplements and food products for a limited number of inherited metabolic diseases. This coverage includes Cystagon for Cystinosis. It is our understanding that individuals with eligible conditions are registered through one of the program’s five regional centres.
89 This information did not soften the blow because, in order to try to explain why others were funded for the drug, the Ministry was for the first time after six months, telling the Comeau-D’Orsays that there was yet another possible funding source, the Inherited Metabolic Disease (IMD) Program, leaving them to wonder why they had not been told before.
(5) Non-Disclosure relating to the Inherited Metabolic Diseases (IMD) Program
90 The Inherited Metabolic Diseases (IMD) Program is administered through the Public Health Division of the Ministry of Health and Long-Term Care. The Program was established well over a decade ago. As its name suggests its general mandate is to determine appropriate strategies and treatment for inherited metabolic diseases. The most recent list of provincially funded treatments and conditions was created on March 1, 2003. It lists supplements and special foods as well as 48 approved drugs. Cystagon is one of 17 Special Access drugs available to patients free through the program, although as mentioned, Cystagon is only approved for the treatment of Cystinosis. This list was compiled by an “Advisory Committee” made up of experts from five regional treatment centres.
91 It is evident that the Inherited Metabolic Disease (IMD) Program is of tremendous relevance in this case. First, Christopher suffers from an inherited metabolic disease. Second, the IMD Program has subsidized the very medication that Christopher needs. Third, this “Special Program” addresses the financial hardship that drugs and food supplement regimes impose for families afflicted with metabolic disorders, the kind of hardship the Comeau-D’Orsays have been living with. Yet when the Director of the Drug Programs Branch responded officially and negatively to Mr. D’Orsay’s desperate plea in November of 2004 no mention is made in her response letter to this Program. And when the government he wanted to help him navigate the network of programs and confusing requirements finally mentioned the Inherited Metabolic Diseases (IMD) Program to Mr. D’Orsay it was not done to assist him in applying. He was told about it in the Ministry’s own interest – as an ineffective attempt to “soften the blow” – to defend its decision by offering some explanation for why Cystagon was funded for some, but not for his gravely ill child.
92 I appreciate that this is a serious charge on my part but I am driven to it. Proof that disclosure was not made in order to assist him by giving him access to one more avenue of recourse is found in a cryptic email prepared on May 3, 2005 after the letter of April 29, 2005 was sent:
The letter that DPB [Drug Program Branch] sent clearly stated that this drug is not covered under ODB. We were vague re: IMD program, because they removed the verbiage that we added directing Mr. D’Orsay to IMD Program. So yes, I think this is in Sandy’s court to respond to as the missing information is the issue that we tried to get her to put into the letter a couple of weeks ago, and there is nothing for us to add (emphasis added).
93 All of this is deeply troubling. Why was there no mention of the Inherited Metabolic Diseases (IMD) Program in his initial letter of refusal, and why was the “verbiage” about the program that would have helped the Comeau-D’Orsays apply omitted intentionally from the April 29, 2005 letter? The evident answer is not a flattering one. It is because the Ministry has allowed the Inherited Metabolic Diseases (IMD) Program to become so degraded that it has been rendered useless in considering new developments and special requests like Christopher’s.
94 When on July 22, 2005 my investigators interviewed Dr. Sandra Bennett, Senior Dental/Child Health Consultant, Public Health Division, she told them that the Advisory Committee for the Program has not operated since 2003. It stopped meeting after the Chair of the Committee resigned and has “basically ceased to function.” There have been no Committee meetings, and for over two years there has simply been no process in place to consider adding new drugs or treatments to the approved list. In a July 25, 2005 internal memo she noted how “Since the Chair of the Committee resigned, PHD [Public Health Division] has been without its process to evaluate new requests for disease, drug supplement and food coverage.” The Program has become so moribund that the Director, Drug Programs Branch, mistakenly told us that the Program had officially ended last year.
95 That this Program has ceased to function effectively is outrageous. On June 28, 2005 Ministry Officials responded to a request for information about funding Cystagon as an “IMD” from the Minister of Health and Long-Term Care Press Secretary. The responding memo said:
Public Health Division has received a number of ad hoc requests for additions to the list of covered drugs, supplements and food products (in addition to those covered by the Drug Programs Branch), as well as diseases/disorders that should be covered. Requests come from staff in the five regional treatment centres, non-specialist health staff, families and advocates. The request for the addition of Batten’s Disease and coverage of Cystagon is one such request. These requests are in addition to the ones that go directly to the Drug Programs Branch of the Ministry.
Rather than review requests on an ad hoc basis, in the absence of an advisory committee the Division has decided to wait until a process has been established to determine how coverage decisions should be made (emphasis added).
96 Frankly, I found all of this breathtaking. An important program was allowed to fall into disuse because of the resignation of its Chair, and as a result, for more than two years there has been no progress made in funding new treatments for metabolic disorders. Special requests for funding initiated by doctors are being shelved and residents of this Province, like Christopher, are let down. They have been left without an effective place to bring their requests for assistance.
97 Consider what happened to Christopher’s request because of the state of this program. In the press fallout surrounding Christopher’s plight the Government began to revisit funding Batten’s Disease treatment as an Inherited Metabolic Disease and whether treatment with Cystagon should be supported. The upshot of its inquiry was simply delay. On June 24, 2005 an electronic message from the Minister’s Press Secretary said:
… I had the feeling in discussing this with Dr. Bennett that if we were to fund treatment of Batten’s Disease as an [Inherited Metabolic Disease] … we would have to await the process being conducted by [Integrated Policy and Planning], which is looking at what diseases to add to those that we are currently screening for. What I need confirmed is whether Batten’s Disease would be among those the advisory committee is even considering.
98 An internal Ministry e-mail dated July 20, 2005 from Dr. Karim Kurji, Associate Chief Medical Officer of Health, which was sent to a number of individuals and copied to Dr. Bennett and others, said:
With the disbanding of the Advisory Committee, there is no current scientific process to evaluate new requests. However IP & P [Integrated Policy and Planning] did call Dr. Chakrobarty at CHEO who indicated Battens disease was a fatal, rather than a treatable condition, and they were left with the understanding that cystagon treatment for Battens disease was experimental.
99 In the absence of a working committee, the extent of Public Health Division medical review for coverage of Cystagon for Batten’s Disease was one phone call. And how focused was this inquiry on Christopher’s case, and how much information about his situation was conveyed, if any? The absence of a functioning committee means that new treatments are not being funded, particular diseases are arbitrarily left without support, and requests for specific relief are either shelved or relegated to the fortunes of inadequate inquiry.
100 What would have happened to Christopher’s request for coverage of Cystagon had it been referred to a functioning Advisory Committee? During the course of this investigation we detected rumblings from some quarters within the Ministry suggesting that it would not have mattered to the outcome – funding would have been denied. On July 21, 2004, a Ministry note, updated four days later, purports to describe the Inherited Metabolic Diseases (IMD) Program. It states:
Children who are identified with a treatable Inherited Metabolic Disease receive follow-up by physicians in one of five specially designed regional centres….
101 On July 11, 2005, during our preliminary inquiries Dr. Bennett suggested to us that Batten’s Disease was not covered by that Program “because it is a terminal disease, it’s fatal and Cystagon has not shown its effectiveness regarding Batten.”
102 I hope that the suggestion made in these communications that treatment for terminal diseases is simply refused summarily under the Inherited Metabolic Diseases (IMD) Program is inaccurate. Such a policy would prevent treatments that could ameliorate or delay suffering. And at what point in the progress of disease treatment does a condition move from “terminal” to “treatable”? What will the long-term fortunes of Christopher be if he remains on the drug? Fortunately, I do not think that it ever was policy to limit funding to treatable diseases. Dr. Bennett confirmed on July 22, 2005 when we interviewed her formally that she did not know if the Advisory Committee had ever been given criteria from the Ministry for making its decisions on funding recommendations, and she indicated that she “certainly never gave them any criteria” even though she was the Ministry contact with the Committee. When asked whether prognosis was an issue considered by the advisory committee, Dr. Bennett replied that the evidence and recommendations were left up to the experts.
103 Leaving recommendations to the experts is sage, particularly in the case of metabolic diseases. Administrators operating general funding programs are accustomed to requests for established treatments for less rarified conditions where scientific support is more apt to exist. As Dr. Clarke, Professor Pediatrics, University of Toronto and Director of the Genetic Metabolic Disease Program explained to my investigators, science is not likely to give a firm answer on many questions relating to metabolic diseases. This is because it is uncommon for metabolic disease research to produce the kind of randomized controlled trials that science is accustomed to. Given the nature of metabolic diseases such trials are not the norm because the diseases tend to be rare and systematic studies are expensive. Dedicated experts in the area understand that a different measure is required. When he was on the Inherited Metabolic Diseases (IMD) Program Advisory Committee that Committee would consider whether a therapy was rational and whether there was good pre-clinical data suggesting it might work. Since the diseases are so devastating, the issue is not so much one of safety as it is where general pharmaceutical marketing is being considered, but rather efficacy. While we can never know for sure, Dr. Clarke was quite confident that the Committee would have approved of funding Christopher’s use of Cystagon and a recommendation would have been made to the Ministry to add it to the list of covered drugs.
104 Without question, the failure to keep the Advisory Committee alive has frozen the Inherited Metabolic Diseases (IMD) Program to the detriment not just of Christopher but of others affected with these horrid conditions. It should not have been allowed to happen and the Government should have been upfront with Christopher’s family about the state of the program.
105 I do not want to leave the impression that this program was functioning effectively before it was allowed to lapse. It is evident from my investigation that, despite the crucial work it performed, the Inherited Metabolic Diseases (IMD) Program had been malfunctioning for some time, even before its disintegration. It was Dr. Clarke, introduced above, who was the Chair whose resignation from the Advisory Committee led ultimately to its collapse. Dr. Bennett’s internal note of July 25, 2005 reports that Dr. Clarke resigned “so he could lobby government for changes around newborn screening and related issues.” He tells us that the reason he in fact resigned was frustration stemming from a lack of a “policy home” for the IMD Program. The Program was managed by the Public Health Division which Dr. Clarke concluded was not particularly interested in its work. His account is supported in a memo of a meeting attended by Dr. Bennett in which his stated reason for leaving is recorded. His account is also supported by Dr. Bennett’s July 25, 2005 memo, which confirms that in 2000 the Public Health Division identified that the Program did not fit within the Division’s mandate, causing the Division to try “to find a more appropriate home for this program component.”
106 Dr. Clarke is clearly frustrated by his experiences on the Advisory Committee. He describes how the Ministry stopped endorsing the Committee’s recommendations because it seemed intent on saving money above all else. Costs had indeed escalated over a decade from $500,000 a year to $3,000,000 because of higher drug costs, patients living longer and the identification of new diseases and treatments, and this would counsel prudence, but we are told it had a completely chilling effect. The point was reached where Committee recommendations were being ignored. It was not that fiscally responsible decisions were being made but rather that responses were unthinking and obstructionist. In one instance the Committee ran into difficulty getting agreement to add a drug name to the approved list, even though the drug had already been approved and what was at issue was a simple change of name. Dr. Clarke resigned because he had had enough of a government bureaucracy willing on the one hand to delegate its responsibility to the Committee to make program management decisions while at the same time ignoring the expert advice of Committee members. Dr. Clarke advised us that while other members of the Committee stayed on for a while, they too eventually left when it was evident the Ministry would take no action on two major recommendations of the Committee relating to drug therapy and newborn screening. Although the Advisory Committee disbanded in 2004, it had been rendered ineffective much earlier than that.
107 So what then is the prognosis for this troubled but essential program? The June 28, 2005 internal memo quoted above records that action on outstanding applications has been left to a program review being conducted by the Ministry’s Strategic Policy Branch of the Newborn Screening Program, in the expectation that this will fix things. We have been told that this review is meant to establish a new process for evaluating which supplements and drugs should be funded. Ms. Carol Apparthurai, Director, Health Information Privacy and Services Branch advised us that this process should be in place by December of this year.
108 It is not my place to tell the Province how to organize itself. It may be that whatever is proposed will bear little resemblance to the Inherited Metabolic Diseases (IMD) Program. What is evident is that this unacceptable lacuna be filled urgently with a process that enables decision-makers to receive expert assistance that is so badly required. A breakdown in government systems cannot be used to justify inertia in matters of life and death.
109 As for Christopher, he and his family were let down by the failure of the Inherited Metabolic Diseases (IMD) Program, by the failure of the Government to be up front about this when confronting his plight, and by the failure to find suitable alternatives for acting responsibly and urgently in his case.
(6) Passing the Buck to the Pharmaceutical Company
110 The last thing that is disconcerting about the way the Comeau-D’Orsays were treated in their attempt to get financial support for their ill son is the repeated suggestions that they throw themselves on the mercy of the drug manufacturer. This kind of advice is found in the last paragraph of the November 5, 2004 response letter, and Mr. D’Orsay was to hear it again from others. He heard it over the phone when he called the Ministry after doing further research in reaction to the initial formal denial of coverage. He was told, “Phone the drug manufacturer and maybe they will give the drug to you for free.” When we began to investigate the Comeau-D’Orsay complaint, Mr. Ron Sapsford, the Deputy Minister, gave us the same advice:
Physicians of patients with Batten’s Disease may wish to continue to work with Health Canada and/or the manufacturer of Cystagon to see if supplies could be obtained on a compassionate basis.
111 The advice that the Comeau-D’Orsays ask the pharmaceutical company to pay was no doubt offered because, in the past, companies have been known to give free medication in special access cases. I understand, however, that this is now happening less frequently. The Director, Drug Programs Branch, advised my investigators that:
“… in the past, typically a lot of these products were given on compassionate ground by the manufacturers and now they’re starting to charge.”
112 What is offensive about the advice that the Comeau-D’Orsays turn to the pharmaceutical company is not so much that such an initiative was likely to end in rejection. It is that the Province was asking the family to engage in a last-ditch exercise without having put adequate effort into seeing what it could do. The government holding responsibility for administering the health care of its residents was sending one of its families off to plead with a manufacturer who bore no legal or moral responsibility to help. To a man whose son’s health is in the balance it must be alienating to be told to rely on the compassion of a foreign commercial pharmaceutical company instead of relying on the compassion of one’s own government. It just seems like one more attempt to pass the buck.
Summary: An Exercise in Bureaucratic Futility
113 It is evident that, altogether apart from the substantive question of whether Cystagon should be funded for Christopher, the Comeau-D’Orsays have not been treated fairly, and their claim has not been given proper consideration. In their attempt to get funding they were passed off, without adequate explanation, to a Federal program. This happened after their desperate claim for financial assistance in maintaining the health of their son was refused, wrongly, on the basis that funding was legally impossible. They met with medical administrators who offered and relied upon different versions of internal government policies, confusing the family as to what they could and should do, and they were led to believe that the particular drug they needed could not be funded by the Province even though the Province was in fact already funding it to treat another condition. They were not told of the existence of the Inherited Metabolic Diseases (IMD) Program, even though it would be precisely the forum for considering their claim, because the Program had been allowed by bureaucratic inertia to fall into a state where it had become virtually unusable. And then they were told to throw themselves on the mercy of the pharmaceutical company. This is a sorry record.
A Bad Policy – How “Approved for Sale” Fetters Ministerial Discretion Irrationally
114 I have already described how the Comeau-D’Orsay family was met with inconsistent policy explanations. I cannot leave my comments at that without examining the policies themselves. Simply put, the “approved for sale” policy is too narrow. It is narrow to the point of being arbitrary. This policy prevents the Province, for largely irrelevant reasons, from even considering reimbursement to Ontario residents for a whole range of prescribed drugs, regardless of efficacy, safety, urgency or cost. Much to be preferred is the “approved for sale or special access” policy.
115 Before making that case in full I want to make clear that I appreciate the need for policies that include a balance between the provision of medical service and fiscal restraint. As a Ministry Backgrounder that was disclosed to us recorded on July 14, 2005:
The introduction of new drugs and increasing utilization of existing drugs are driving program costs.
The government is committed to supporting drug benefit programs that take a balanced approach that is fiscally responsible yet addresses the needs of the most vulnerable.
116 I am sure that all residents of this Province appreciate that any commitment to medical services must be a fiscally responsible one. I hasten to add, however, that they would not likely support an arbitrary disqualification of meritorious claims to save money. They would want monetary decisions to be tied to other criteria that would enable the rational identification of priorities.
117 I also appreciate that this case illustrates another concern that can and should influence funding decisions. Desperate families often resort to untried treatments, even leaving the country as the Comeau-D’Orsays did. Not infrequently families turn to less highly regulated places than the United States to receive experimental or even unconventional and highly speculative forms of therapy. Their desperation can lead to an irrational belief in the promise a treatment holds out and then to insistence on government support and righteous indignation when it is not forthcoming. Responsible policy must protect valuable health care dollars from being squandered because of sympathy, when medical indications cannot justify the expenditure. I understand this. No medical expenditure should be funded pointlessly out of kindness or misdirected compassion.
118 Perhaps the key to understanding why the “approved for sale” policy is inappropriate for section 8 is to bear in mind the discretionary nature of section 8 applications. Section 8 of the Ontario Drug Benefit Act provides for case-by-case relief. As a Ministry Backgrounder explains:
The Section 8 mechanism is designed to provide access for ODB-eligible persons, on a case by case basis, to unlisted drugs where listed drugs have been tried and are ineffective or not tolerated, where the patient does not meet the clinical criteria for the listed drug or when there is no alternative available on the Formulary.
119 When we interviewed her, the Director, Drug Programs Branch, explained the provision this way:
The individual clinic review we do, what we call section 8, has been our safety valve, it’s where a drug has been reviewed by the committee, not listed, but we recognize there might be individual circumstances where a person absolutely needs to have the medication….
120 Quite clearly, the provision exists to enable funding to be provided in specific situations of demonstrated need where the spirit of the Ontario Drug Benefit Act is met, i.e., where those burdened with their legitimate medical need for the drug are either elderly, poor, institutionalized, or burdened with crushing or inordinate drug costs. Imposing rigid preconditions to even considering an application defeats the purpose behind the provision. If an imposed and rigid precondition is not met, then no funding is possible no matter how medically necessary the drug might be or how crushing the financial burden on the patient is. In contrast, removing the rigid precondition enables all cases to be considered on their merits while continuing to empower decision-makers to refuse funding where it is not appropriate.
121 To make the point more concretely, focus on the “approved for sale” policy and take this case as an example. The Director, Drug Programs Branch, acknowledged when we interviewed her that in denying Christopher’s claim according to this policy the Ministry did not consider the medical evidence supporting Christopher’s medical need to continue to receive Cystagon, or the irrefutable evidence that it is having remarkable results in his case. She admitted that the Ministry not only failed to consider this overwhelming human dimension but that it did not even consider cost effectiveness – that without Cystagon Christopher’s condition would deteriorate to the point where he would require institutional care at far greater cost to the public purse. As a result of this discreditable policy, when Christopher’s individual needs were being evaluated under a regime intended to make discretionary case-by-case decisions, he was denied coverage because his case did not fit into a pre-ordained box, the “approved for sale” list established by the Federal Government. Worse, that pre-ordained box was designed to deal with a different question – not with Christopher’s welfare and medical needs but with marketing of drugs at large. Christopher’s fate was effectively delegated to another government’s decision-maker who was making a decision on issues different from the ones Christopher faced. Why on earth would anyone seek to fetter a program intended to enable specific, case-by-case assessments with the requirement that generalized approval to sell the drug be obtained first? As I say, it defeats much of the purpose of section 8 to do so.
122 The July 14, 2005 Backgrounder referred to above, which wisely reminds its readers of the need to consider program costs and to be fiscally responsible, also carries this claim:
The Ministry is continuing to examine ways to improve utilization by ensuring that prescription drug benefits are consistent with up-to-date clinical and cost-benefit evidence.
123 I do not see that objective being served by the “approved for sale” policy. This policy prevents the consideration of “up-to-date clinical” evidence in cases in which manufacturers who possess such proof choose, for commercial reasons, not to seek general marketing approval. According to the “approved for sale” policy the Minister should not have the power to fund Cystagon even for Cystinosis patients despite that it is a legal drug and the routine treatment for the disorder. The policy discriminates against those afflicted with rare conditions. Under it the fortunes of residents of Ontario would turn on whether the medical condition they are afflicted with is common enough to be a profitable market for drug manufacturers. There is something more than a little unsettling about this.
124 As for “cost-benefit” objectives, I have already addressed the point; Christopher’s condition will cost less to treat with Cystagon than if he is medicated for his symptoms alone and left to degenerate to the point where he finds himself institutionalized.
125 Simply put, the “approved for sale” policy is an unthinking one. It throws out the baby with the bathwater. By contrast, the “approved for sale or special access policy” enables anyone who needs drugs in this Province to make a case on its merits, first to a federal body, and if successful, to an expert provincial body capable of making contextual and rational decisions.
126 I understand how burdened the section 8 administrators are – how their caseload has grown over time from a few hundred cases a year to hundreds a day. Arbitrarily confining its mandate to commercially viable drugs that are measured only for their general efficacy and relative safety rather than according to the needs of specific cases is not a fair way to cope with the overload. The “approved for sale” policy cannot be justified.
Solutions
127 I have both individual and systemic solutions to offer. The first is obvious. Fund Christopher’s medication. Help to save the boy and his family from emotional and financial ruin. The case for doing so is overwhelming.
- The drug is legal;
- While its application in his case is new, the drug itself is not experimental and has been approved generally for sale according to FDA standards and is authorized for the treatment of another condition in Canada;
- It is prescribed by his treating physicians as not only the best but the only possible treatment for his disease;
- Even though there is inadequate clinical information to enable science to prove that Cystagon is a benefit for Christopher’s form of Batten’s Disease generally, this is because the disease is rare and the drug’s applications are not considered by the manufacturer to be commercially viable. The only evidence generated, even though anecdotal, demonstrates overwhelmingly that Cystagon has improved Christopher’s condition and that without it he will die;
- His parents are met with the kind of crushing drug debt that the Trillium Drug Program and Inherited Metabolic Diseases (IMD) Program are meant to ameliorate;
- Funding this medicine may save the Province money that would otherwise be spent on ineffectual treatment and institutional care; and
- There is no policy based need to require this boy to suffer and die to prevent abuses of healthcare funding in the future, as his funding would be a discretionary, case-by-case decision justified on the particular evidence.
128 It would be possible, of course, if the “approved for sale or special access” policy is applied to have Christopher get approval from the Federal Special Access Programme and then resubmit his claim to the Trillium Program where it can be re-evaluated, free from the process-based errors that have tainted the initial refusal. I am rejecting that as a recommended solution in this case for four reasons:
- His receipt of the drugs is already in compliance with Federal access rules and it would be redundant to require him to receive additional approval under the Special Access Programme;
- The Province of Ontario is, at present, ill-equipped to assess a claim related to a rare metabolic disease properly because of the failed “Inherited Metabolic Diseases (IMD) Program”;
- The Comeau-D’Orsay family has been at this long enough. They have butted heads with medical administrators who did not know the rules, or even their own policies, and who have created the real impression that their task is to find ways to justify refusing coverage rather than to find ways to help a family in need; and
- Retroactive reimbursement back to the time the Comeau-D’Orsays originally applied for funding is in order, and sending the family through the Special Access Programme and then the Trillium Drug Program will not achieve this.
129 I am recommending that the Minister use his special or inherent power to authorize this expenditure in the interests of Christopher’s health and welfare.
If and when Christopher is unable to secure Cystagon in the United States in connection with the clinical project he will have to secure Special Access Programme approval to enable the Province to continue to fund him.
130 The second solution is to immediately clarify and publish a policy within the Ministry authorizing consideration under section 8 of the Ontario Drug Benefit Act of requests for benefit coverage for drugs obtained under the Federal Special Access Programme, in addition to drugs that are approved for sale in Canada.
131 The third solution is to act with urgency in reinvigorating the Inherited Metabolic Diseases (IMD) Program, or in developing a successor program. Cumulatively, there are many people in this Province who are suffering from metabolic disorders, some of them readily treatable. It is a slur on the Ministry that this program has failed not because of rational, medical or resource-based decisions but because of structural uncertainty about where the program should be housed and because of a malfunctioning relationship between an advisory board and bureaucrats who were frozen by fiscal obsession.
132 Accordingly, I have reached the following opinions and recommendations:
Opinions
Opinion 1
The Ministry of Health and Long-Term Care’s failure to fund Cystagon for Christopher Comeau-D’Orsay is unreasonable.
Opinion 2
The practice within the Ministry of Health and Long-Term Care of confining its consideration of drugs under s. 8 of the Ontario Drug Benefit Act to those that have been approved federally for sale is unjust.
Opinion 3
The Ministry of Health and Long-Term Care’s omission to actively address issues relating to the Inherited Metabolic Diseases (IMD) Program in the last few years is oppressive and wrong.
Recommendations
Recommendation 1
The Ministry of Health and Long-Term Care should fund Cystagon for Christopher Comeau-D’Orsay and pay retroactively for the costs incurred by his family from the time of their initial application for subsidy.
Recommendation 2
The Ministry of Health and Long-Term Care should either clarify or change its policies to ensure that requests for drug funding can be considered under section 8 of the Ontario Drug Benefit Act for drugs authorized under the Special Access Programme as well as drugs approved for sale in Canada.
Recommendation 3
The Ministry of Health and Long-Term Care should take all necessary steps to ensure that the Inherited Metabolic Diseases (IMD) Program, or a successor program, is actively engaged and operating effectively.
Ministry's Response
133 On August 19, 2005, I delivered my Preliminary Report to the Ministry, setting out my preliminary findings, opinions and recommendations. On August 29, 2005, Mr. Ron Sapsford, the Deputy Minister personally attended at my Office to deliver the Ministry’s official response. He articulated full support for my Report. In a letter he presented to me he noted:
The Ministry of Health and Long-Term Care recognizes that, had the Advisory Committee on Inherited Metabolic Diseases been functioning at the time of the D’Orsay family’s initial application, the result of that application may have been different. Given this fact, together with other arguments raised in your analysis and advice, the Ministry agrees to fund Cystagon for Christopher Comeau-D’Orsay, effective immediately, and will, in this case, pay retroactively for the cost of the drug incurred by his family from the time of their initial application for funding, as you have recommended.
Another issue that you raised deals with the section 8 application process and current ministry policy. In June of 2005, the Ministry established a Drug System Secretariat, to develop, consult, recommend, and implement system-wide changes that would create positive outcomes for patients within a sustainable system and accountable to Ontario taxpayers. Strategies to address several of the issues raised in your Report, including the section 8 process of the Ontario Drug Benefit Act (ODBA), are under consideration for change.
The Ministry will move expeditiously to develop a new protocol for responding to requests for funding under the ODBA. This will include clear statements as to the process and criteria for funding approvals. Where other programs or services exist that would assist patients, these will be clearly identified at that time.
With respect to the Inherited Metabolic Diseases (IMD) Committee, the Ministry will move immediately to put into place a new process that will take on the major responsibility of the former IMD Committee. This will allow the Ministry to respond to these types of applications in the future. This action is intended to be in compliance with your recommendations.
I sincerely regret the difficulties the Comeau-D’Orsay family encountered in their efforts to obtain funding for Christopher.
While not evident in the Report, I can assure you that the Ministry and its staff try hard to be conscious of the needs of Ontarians. This is a Ministry that strives for quality in its services and is quick to respond to errors. Your report has helped to clarify a number of programs and policy inconsistencies that the Ministry will move to correct.
134 I commend the Deputy Minister for taking positive steps to address the issues highlighted in my Report. The Ministry’s acceptance of my recommendations demonstrates a strong commitment to fairness and accountability within government and to the public of Ontario.
______________________
André Marin
Ombudsman of Ontario
[1] One group of “eligible persons,” not relevant to this Report, are “seniors, those on social assistance and professional home care services, and residents of long term care and special care facilities.” They are eligible under the “Ontario Drug Benefit (ODB) Program.”
[2] I am not clear whether the “Trillium Drug Program” is part of the “Ontario Drug Benefit Program,” or independent of it – Ministry documents uncovered in our investigation vary in this regard. The correct characterization does not matter, although it is important to note that in the correspondence sent to the Comeau-D’Orsays, reference to the “Ontario Drug Program” is treated as including the “Trillium Drug Program.”
[3] This comment, which implies inaccurately that Health Canada has refused to approve Cystagon as treatment for Batten’s Disease, is based on a misreading of Mr. D’Orsay’s letters. He never said that Health Canada refused a Special Access Program request related to Batten’s Disease. He simply said, “[W]e are unable to obtain Cystagon in Canada because it is a special-access drug only prescribed here to treat Cystinosis.” The reply letter was based on a misunderstanding of the facts that could have been avoided with a little research.
[4] This possibility emerged because Mr. D’Orsay does indeed ask in his letter for help in obtaining access to the drug in Canada, a request he made because he had to purchase the drug in the United States.
[5] Indeed, as discussed below the Province was funding Cystagon, but only for Cystinosis patients.
[6] To be fair, I have to allow for the possibility that letter is technically accurate because Cystagon is supplied to Cystinosis patients under the IMD Program and the letter says it is not eligible under the “Formulary or … ODB program.” Unfortunately I am left uncertain from inconsistent Ministry documents whether the IMD Special Program shelters under the ODB program or is separate from it. If the IMD Special Program is not part of the “ODB program” the representation in the letter is technically accurate. In the end, I think that little turns on it. Either when she signed the letter the Director of the Drug Programs Branch did not know that Cystagon was being funded under the IMD Special Program or she was content that the letter be worded strategically to create the impression that the drug could not be paid for by the Ministry. I have no evidence to suggest that the Director would have tried to mislead the Comeau- D’Orsay family in this way. Indeed, I believe that she was being honest when she told us mistakenly that if Cystagon is being paid for by the Ministry it must be out of hospital budgets. I am therefore proceeding on the footing that this was a case of her not knowing about a fact and representing the contrary without her staff having done the proper homework. Either way, the representation should not have happened.